References
Reflections on twelve years of breakages – lessons to be learnt
From Volume 10, Issue 4, October 2017 | Pages 140-145
Article

Breakages and emergency appointments disrupt the clinical management of patients during treatment, incurring administration time and expense. In 2004, the author visited a colleague in another hospital and noticed a ‘breakage book’. This seemed an excellent idea in order to keep a record of all patient/appliance-related emergencies. It is not easy to improve any aspect of clinical practice until the nature and extent of the problem has been determined.
Audit aim
The aim of this project was to record all breakages, whether at routine or emergency appointments and then use the first year's figures hopefully to reduce the failures and emergency attendance rate year on year.
Method
The following data were recorded:

All teeth, including molars, were routinely bonded; bands were only used on teeth that required auxiliaries such as a lingual or palatal arch. All teeth showing bracket failures were re-bonded with a new bracket. Bands were not used to replace debonded brackets or tubes; the tooth was re-bonded.
Brackets that needed repositioning were removed with a 3M Lift-Off™ tool (Figures 2 and 3) to prevent any damage to the bracket base. The bracket was then cleaned with acetone and re-bonded with 3M Transbond XT™, providing that there was no composite left on the bracket base (Figure 4). If composite was evident on a bracket base a new bracket was used.



For a short time, an attempt was made to record the total number of brackets/tubes in place on all the patients to allow calculation of a percentage failure rate. This figure constantly fluctuates with the proportion of extraction cases, bond placements and debonds, so it was quickly apparent that this was not practical for this type of rolling audit. The clinic patterns, time worked and number of patients under treatment, approximately 200, has not changed significantly year on year during this audit so the ‘bottom line’ is the actual number of emergencies and breakages that have to be treated annually. Only the author's patients under active treatment were included; there were no exclusions.
The data were complicated by two confounding factors over the long period of this audit. Self-ligating brackets (3M Smartclip™) and 3M self-etching primers were introduced in 2007, resulting in all patients being treated with both. As the results of this audit unfolded, a decision was made to revert back to conventional brackets (3M Victory Low profile MBT™) and conventional etching. The tubes used on molar teeth have remained of constant make and design (3M) throughout the audit, until September 2015 when a new design of 3M first molar tube was introduced.
The data used were recorded from June 2004 until June 2016 and are still being recorded to date.
Results
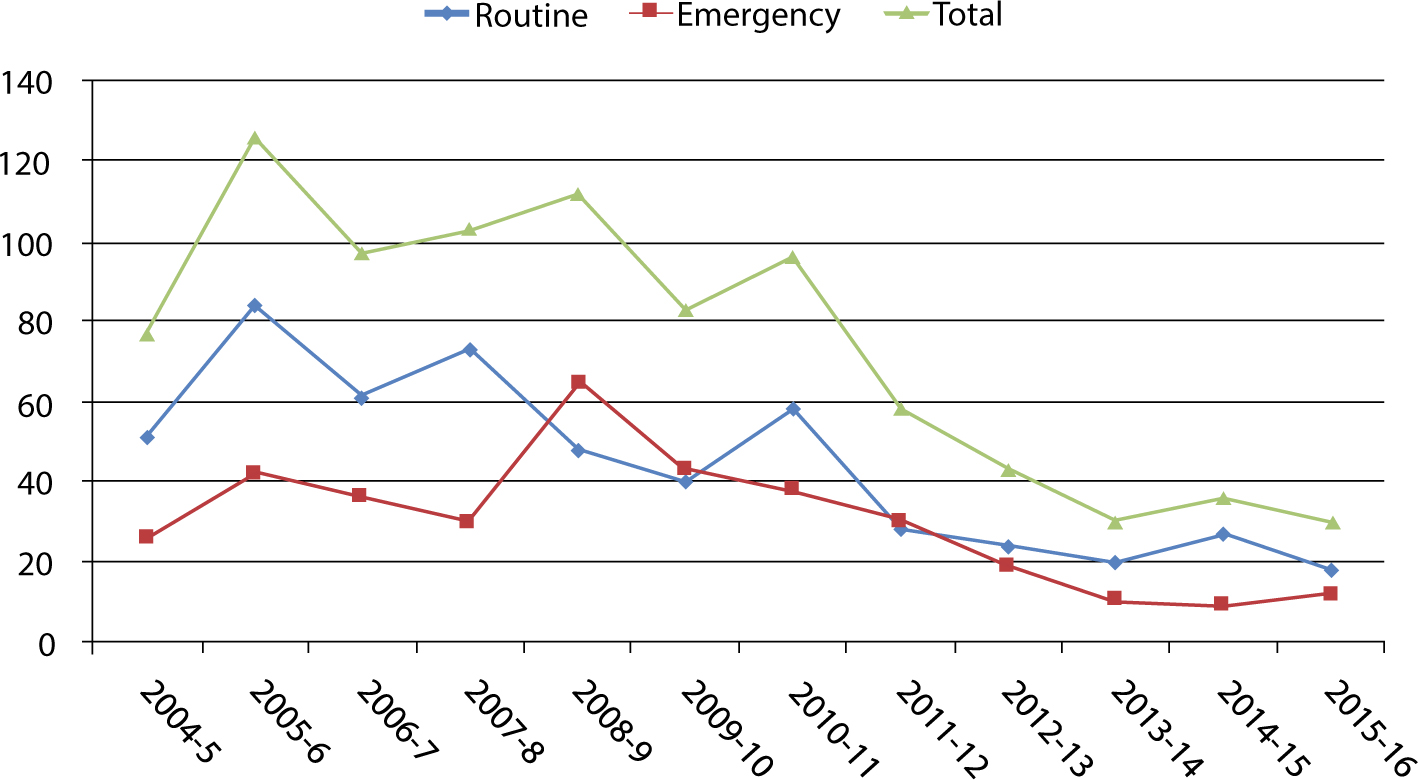
The data have been separated into total emergency appointments, bracket failures and miscellaneous problems (Figure 5). After the first year, 2004, the totals increased in 2005 and then steadily decreased for two years. Following the introduction of self-etch primer (SEP) and self-ligating brackets in 2007/8 the total climbed to a peak in 2008/9 before gradually decreasing again to 2016 as the practice changed back to conventional brackets and etchant.
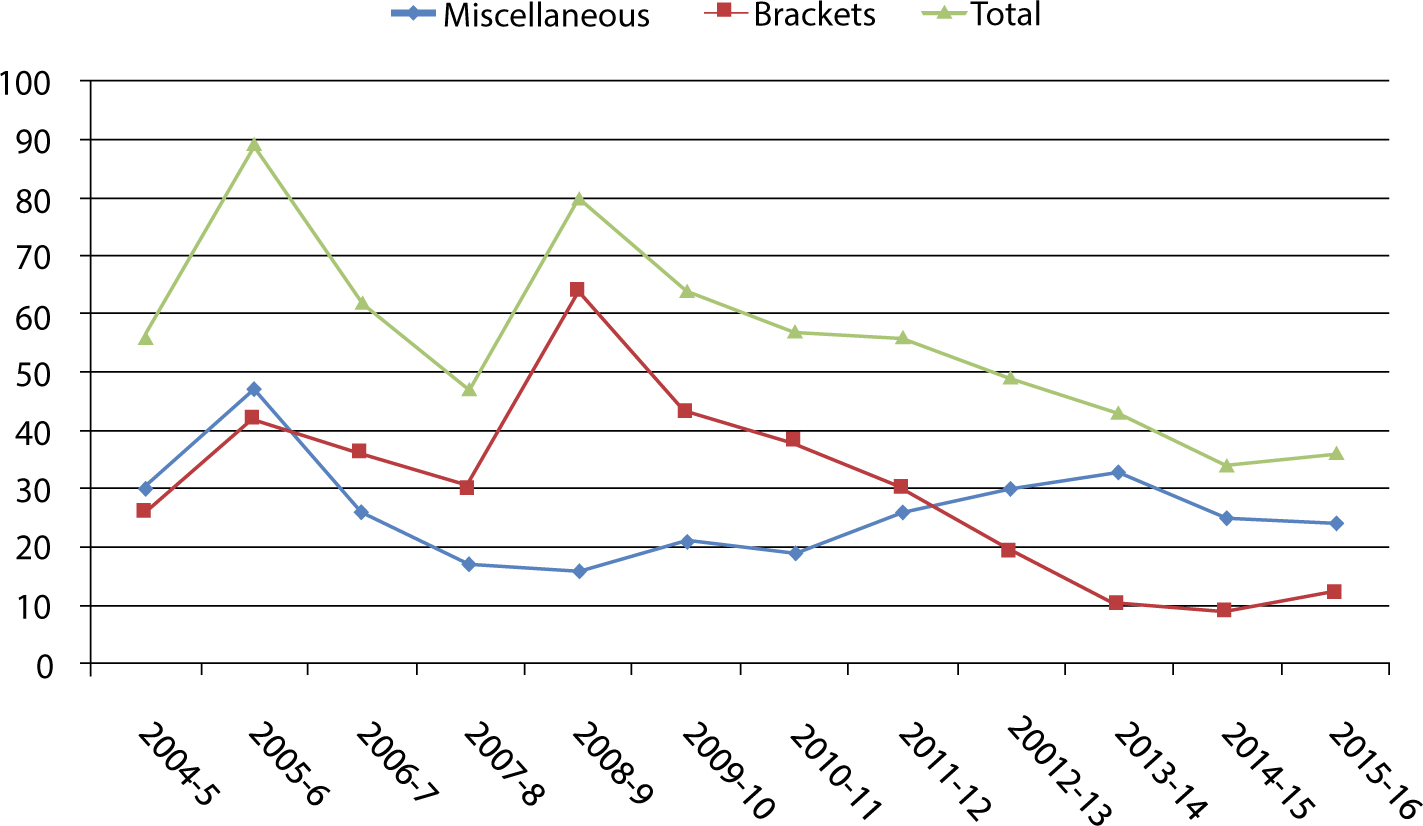
Bracket failures found at routine appointments remained higher than those presenting as an emergency in all but two years, 2008/9 and 2009/10 (Figure 6). This may have been caused by a change in the site of bracket failures (Figure 7).

More anterior brackets failed in 2008 which coincides with the greatest number of emergency appointments shown in Figures 5 and 6.
It can be seen in Figures 8 and 9 that the proportion of the breakages where the bracket failed between the bracket and adhesive and at the enamel surface varied.


Only in 2005/6 did the ratio of failures that might be considered operator error fall below those where the patient or bracket base may be responsible; both values were high. The decision to record composite either present or not on the enamel surface judges the failures more harshly than might have been apparent had an ARI index been used. Over the total audit, 63% of failures occurred at the composite/enamel interface.
The greatest number of enamel interface failures occurred in 2008/9, which coincides with the highest incidence of anterior bracket failure, overall bracket failure and total number of emergency appointments (Figure 10).

From 2008 to 2016 the total number of brackets broken reduced by 70.8%, those at the adhesive/enamel interface by 76% and at the adhesive bracket interface by 63%.
Discussion
Despite the apparently small number of factors recorded, it was surprising just how much information can be analysed. Using a simple set of data prevented fatigue in collecting it over the long period of the audit. The data were easy for the nurses to record if the patient was not seen by the author. Any breakage in the notes seen by another operator was checked as being present in the breakage book, the vast majority of repairs were carried out by the author.
The total number of emergency appointments increased during the first year of the audit due to a 63% increase in bracket failures. No changes in clinical practice or materials occurred during this year; the cause for this was unclear at the time and was certainly unexpected. Having studied this data, more care, but no additional other measures were taken over the bonding procedure. The next two years brought slight improvements.
In 2008–9 emergencies increased again and this was due to a large increase in bracket failures; miscellaneous problems were not significantly different. The site of failures also changed with the introduction of self-etching primer and self-ligating brackets; more brackets failed at the enamel composite interface (Figure 9). It was also noticeable that bracket failures in teeth that had previously been less common, such as incisors and canines, increased (Figure 7). To begin with it was not clear what was causing the failures to rise. Both self-ligating and conventional brackets were pre-coated with the same adhesive, 3MTransbond™,TM which remained constant throughout the audit. The self-etchant instructions were closely followed and more rigorous cleaning of enamel surfaces was carried out using an ultrasonic scaler and non-fluoridated oil-free prophylactic paste. Despite this attention to detail, the bracket failure rate continued to be unacceptable.
In 2010, the author decided to return to solely using conventional brackets and etching for all patients owing, in part, to the higher failure rate. Any rare use of self-etch primer for ectopic teeth or a repair was subsequently noted. By 2012, there were very few patients with either self-ligating brackets in place or for whom SEP had still been used in treatment.
To improve bonding reliability, the following additional measures were introduced in 2011:
Bracket failures have steadily reduced since 2008 with an overall 73% reduction between 2008 and 2016 (Figure 10). It is not possible to determine whether changes in enamel preparation and moisture contamination, or the bracket and etch type, played the greatest role. The reduction of 76% of enamel/composite failures would suggest that cleaning the teeth more rigorously has been effective.
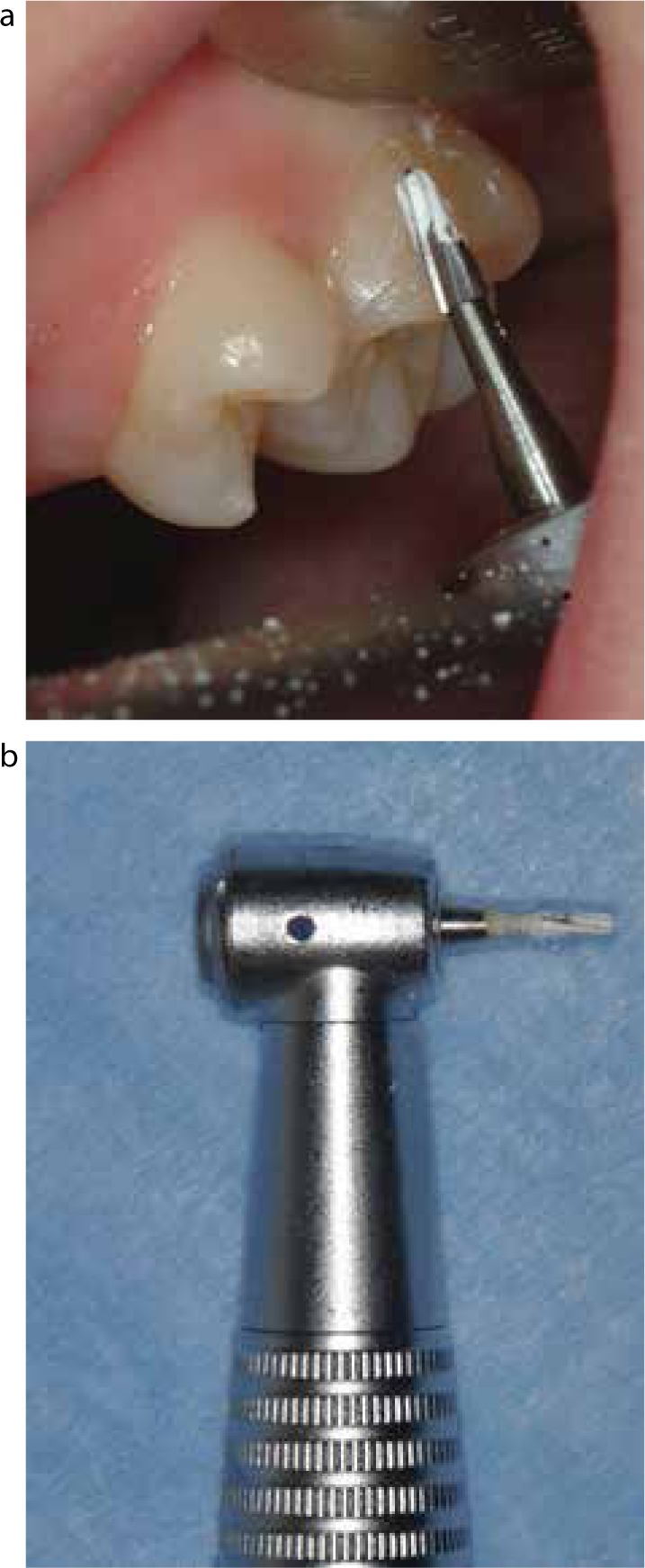
Cleaning the teeth routinely with the tungsten carbide bur improved the etch appearance. The ultrasonic scaler was not effective at cleaning all the debris, leaving marks within it. When cleaned with the bur, the enamel is transformed (Figure 14). The amount of debris removed with the bur is surprising, even on apparently clean teeth (Figure 15). The upper molars are often affected by a thin layer of calculus from the parotid duct. Teeth displaced from the dental arch and out of reach of careful brushing also gain calculus and need cleaning. A pure air source visually dries the teeth much more effectively. Primer rapidly disperses away from the micro-brush in a capillary action. Mixed air/water syringe tips often need clearing of water. Despite trying several types of syringe tips from different manufacturers, none provided completely dry air. Disconnecting the water is easy and cheap to change on any dental unit. Most units have two ‘three-in-one’ syringes so one can be used for water, the other for dry air.
A randomized clinical trial,1 comparing SEP and conventional etching, found an increased clinical bond failure rate using SEP. A systematic review,2 comparing self-etch and conventional acid-etch primers, concluded that there is weak but statistically significant evidence indicating a higher chance of failure with self-etch primer. Due to both an increase in bracket failures and the change in proportion of failures at the composite-enamel interface, this conclusion is reflected, but not confirmed, in this audit.
Re-bonding the same bracket after re-positioning, providing the mesh is clean of composite, did not result in increased bracket failure during this audit. The Lift-Off™ tool does not damage the bracket base or wing on debonding. Since the patient's name for each failure was recorded, these re-positioned brackets could be followed.
Over the twelve years of the audit, bracket failures have reduced by 61% but this has been a Pyrrhic victory due to the high failure rates in the intervening years. The overall reduction of 61.5% in emergency appointments has been extremely beneficial; there are far fewer bracket failures as a proportion so that these appointments are less time consuming (Figure 6).
It is noticeable from the data that a small number of patients cause the greatest number of breakages. During the last year of the audit, one orthognathic patient with learning difficulties fractured six attachments, 20% of the total bond failures.
Miscellaneous emergencies were dominated by wire trauma, three of the four most frequent miscellaneous emergencies (Figure 11). Wires are routinely annealed and tucked in. Crimpable stops are used where necessary. Wires out of tubes are often associated with losing an elastic ligature on a lower second premolar. Where the occlusion is traumatic, a wire ligature on the bracket is helpful and wire emergencies in general have been reduced by using wire ligatures more often at strategic points. When appointment intervals are too long during space closure, wire protrudes behind molar tubes, leading to discomfort. Most patients have second molar tubes which increases the risk of wire trauma.
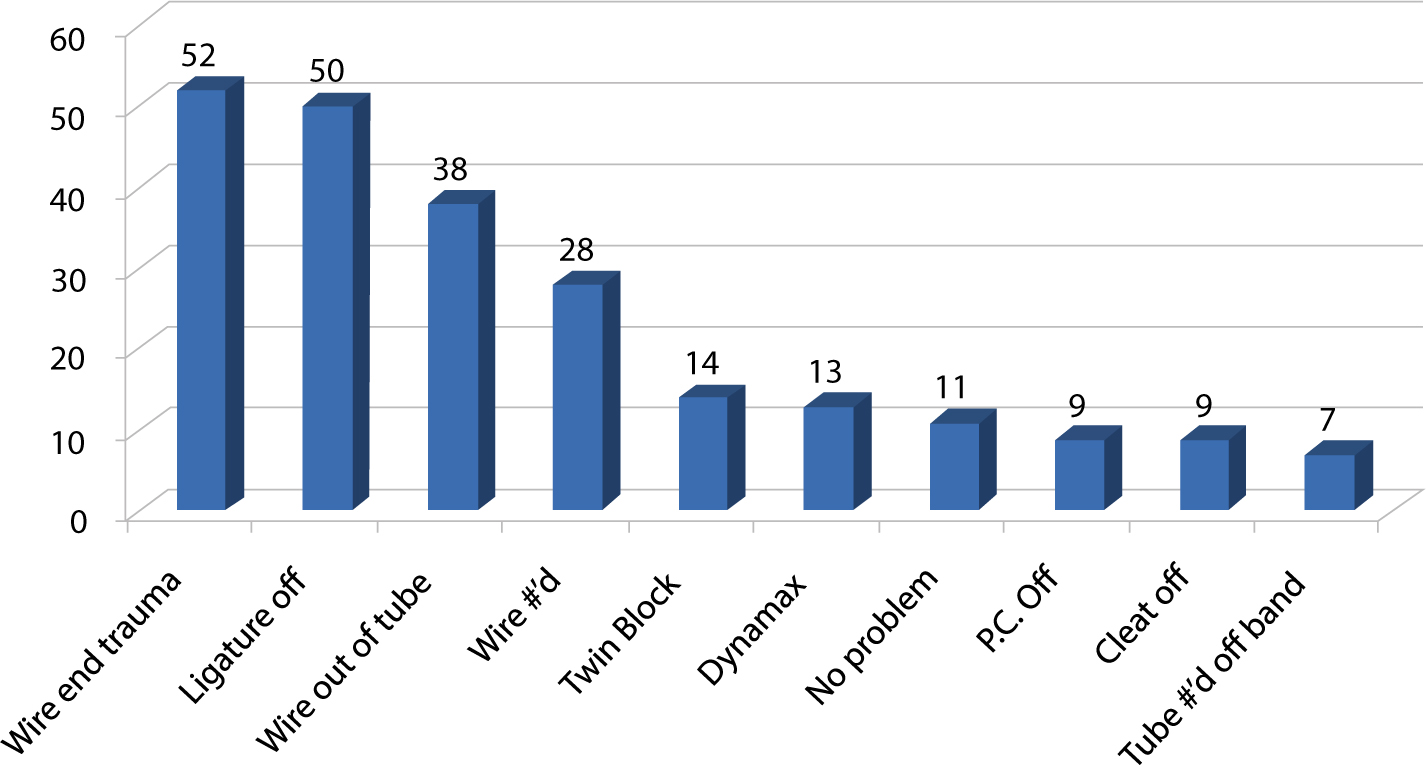



Twin blocks are made with 0.8mm wire and no vertical tags of wire in the acrylic so that breakages are rare. The Dynamax appliance features, despite the very short time it was used.
Tubes fracturing off bands were almost always due to incomplete welding when the laboratory chose the bands for auxiliaries.
Although it surprising to see ‘no problem’ featuring in the top ten categories (Figure 11), this only equates to one patient visit a year.
