Abstract
Failure of eruption (FOE) of first and second permanent molars is rare, with an estimated prevalence of 0.01% in the case of the first permanent molar and 0.06% in the case of the second.
From Volume 11, Issue 4, October 2018 | Pages 133-138
Failure of eruption (FOE) of first and second permanent molars is rare, with an estimated prevalence of 0.01% in the case of the first permanent molar and 0.06% in the case of the second.
Primary failure of eruption (PFE) is an isolated condition causing a localized failure of tooth eruption with no other identifiable local or systemic involvement. It is rare, with an estimated incidence of 0.06% with a gender ratio of 2.25:1 (F:M).2 It has been described based upon the following clinical features:3
Frazier-Bowers et al described three different forms of PFE:4
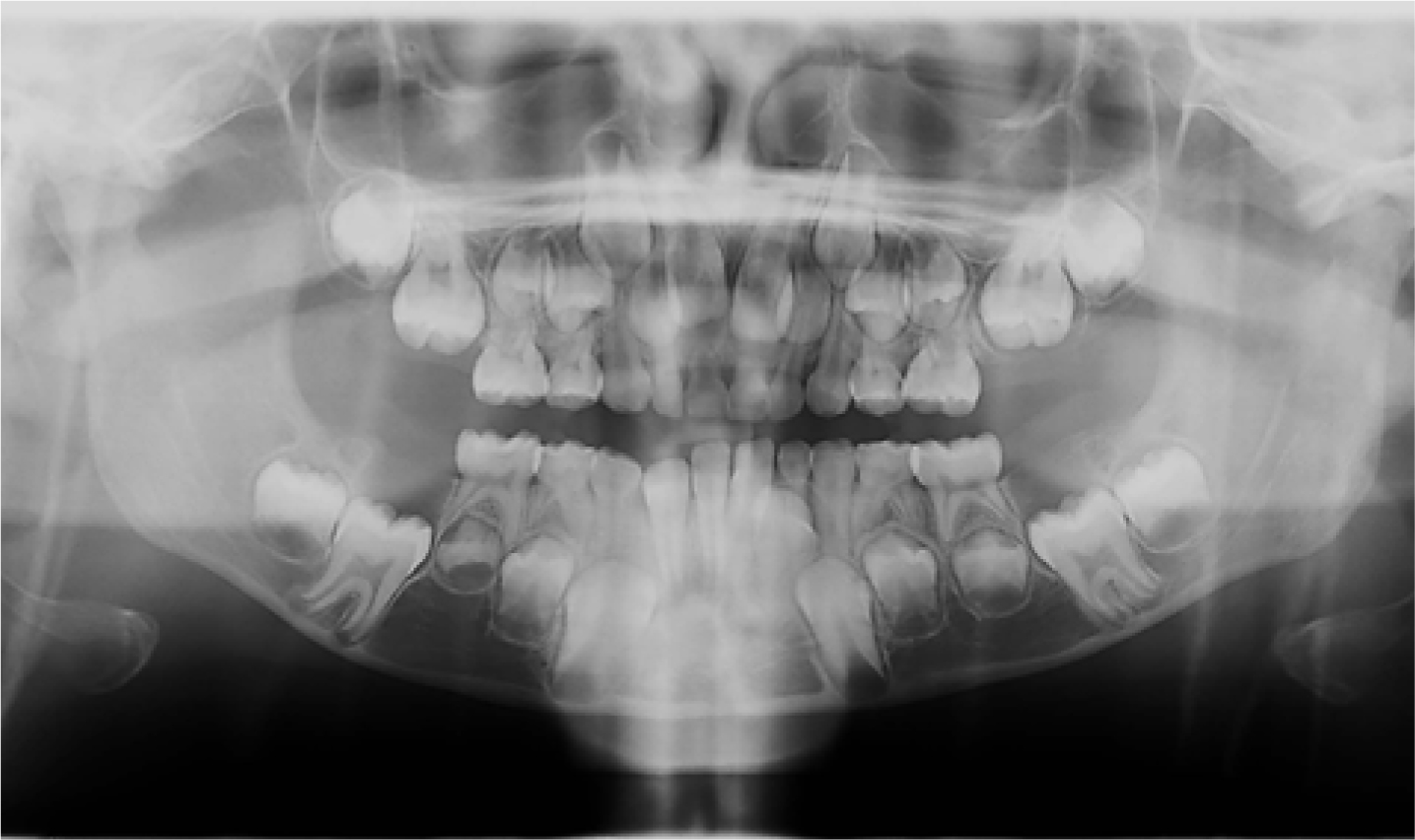
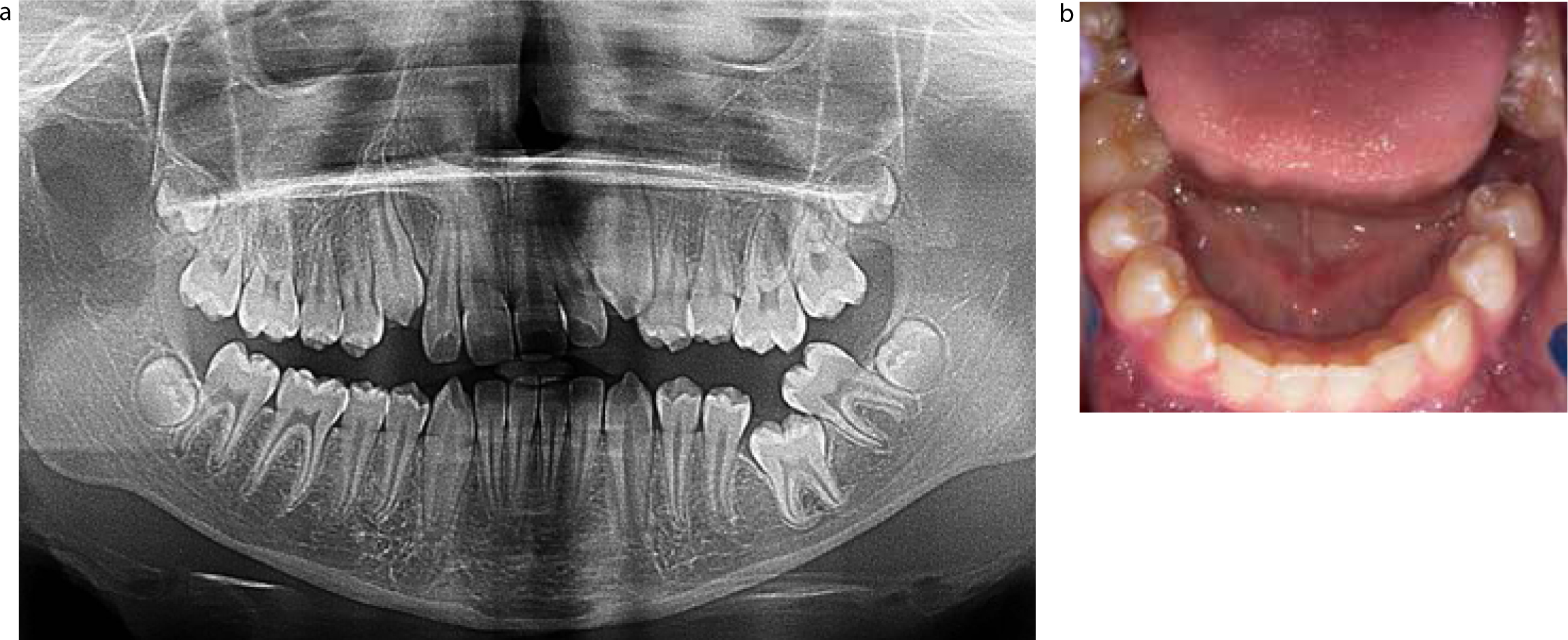
Radiographically, full root development is seen and the tooth is normally orientated in the eruption path.5 There is no evidence of any obstruction, eg overlying bone/pathology associated with the teeth which have failed to erupt. There will be evidence of bone resorption supra-coronally, giving rise to the classical ‘chimney’-like appearance6 (Figure 1) over the lower first permanent molars only. This appearance suggests a normal resorption process and deficiency of eruptive force to move the tooth along the path of eruption. Figure 2 is another example of a patient with PFE affecting the upper left first and second permanent molar teeth.

The aetiology of PFE is complex. Evidence from the literature indicates that this disorder has a strong genetic component. A positive family history has been found in many studies.7,8,9-10 PFE has an autosomal dominant inheritance pattern. Heterozygous mutation of the parathyroid hormone 1 receptor (PTH1R) gene has been shown to cause PFE, likely due to protein haploinsufficiency.11 However, Jelani et al report upon PFE caused by homozygous mutation of PTH1R in four members of the same family.12
Recent studies have shown that a genetic mutation in the PTH1R gene is associated with PFE, where the mutation is present in multiple numbers of some families.11,13,14 In this regard, a positive family history +/- confirmed mutation of the PTH1R gene can be used to aid diagnosis of PFE. Further, an association between PFE with dental anomalies of known genetic origin would also suggest that PFE has a substantial genetic component.15 For example, Mattheeuws et al found the level of hypodontia to be considerably higher in the PFE population at 13% than that of the normal population (5%).16 Hormonal disturbances or developmental syndromes, such as cleidocranial dysplasia, osteopetrosis and GAPO syndrome, have also been associated with PFE in which abnormal eruptive mechanisms can delay or prevent tooth eruption.17
Single tooth ankylosis/MFE is a rare condition with a similar presentation to PFE. A key diagnostic feature distinguishing PFE Type II from MFE is that MFE often only affects a single tooth and teeth distal to that are not affected. This is difficult to diagnose in a young child, as it is impossible to determine whether all of the teeth distal to the first permanent molar will suffer the same fate. Clinically, where a tooth is partially erupted, the percussion test can be carried out and a tooth affected by MFE is likely to exhibit a dull metallic sound on percussion.18 Adjacent teeth may tilt into the space and opposing teeth can over-erupt (Figure 3). Radiographically, there is the appearance of relative submergence due to ankylosis. A focal obliteration of the periodontal ligament space or resorption of the root surface may be seen, although this may not be obvious radiographically, as it may occur on the buccal or lingual aspects of the tooth, or because it occurs minimally on the mesial and distal aspects.19 Additional dental anomalies, such as hypodontia, hypercementosis, cementoma and sclerosed roots, may also be present.20,21,22,23
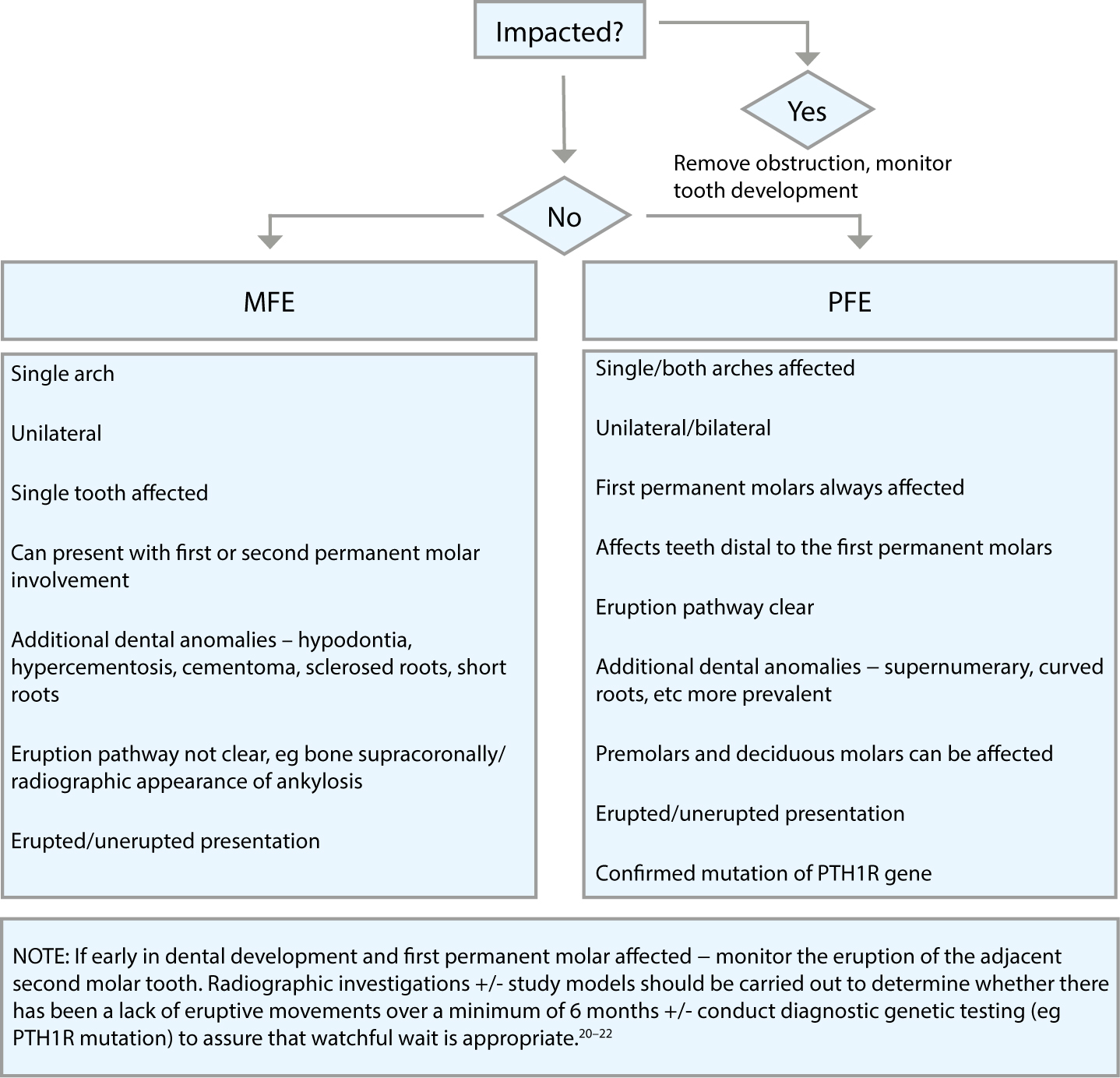
Accurate diagnosis of failure of eruption is challenging; with evidence that PFE is sometimes misdiagnosed as MFE.20 Both conditions affect the first permanent molar, which can be supracrestal/infracrestal in presentation. Limited studies have proposed protocols for the management of failure of eruption of permanent molars with no clear consensus or guidelines. Sharma et al carried out a retrospective descriptive study to establish a diagnostic decision tree to aid diagnosis and management of failure of eruption.23 This involved identifying patients with failure of eruption of permanent molars attributed to PFE or MFE due to ankylosis via a combination of published protocols and guidelines outlined in Table 1. Based on the results of this study, a flow diagram was formulated to aid diagnosis of failure of eruption of permanent molars (Figure 4).
| Features | Diagnostic Criteria | PFE I | PFE II | MFE |
|---|---|---|---|---|
| Clinical | Permanent molar affected | 1st molar always | 1st molar always | Either 1st or 2nd molar |
| Teeth distal to most mesial affected | Yes | Yes | No | |
| Deciduous dentition affected | Possible | Possible | No | |
| Multiple teeth | Possible | Possible | No | |
| Position of tooth | Infra-crestal | Supra or infra-crestal | Supra or infra-crestal | |
| Quadrants involved | Single/multiple | Single/multiple | Single | |
| Posterior/lateral open bite | Yes | Yes | No | |
| Percussion test | N/A | Can be +ve | +ve | |
| Radiographic | Eruption pathway | Clear | Clear | Not clear eg overlying bone |
| Other | Response to treatment | Unsuccessful orthodontic extrusion | Unsuccessful orthodontic extrusion | Successful luxation and subsequent extrusion of tooth Extraction of the tooth in question and successful eruption of all teeth distal |
Early distinction between MFE and PFE is important in the management of patients with failure of eruption of permanent molars since they dictate different treatment modalities. MFE is often successfully treated via the extraction of the affected tooth at the appropriate age, or occasionally luxation of the affected tooth and subsequent orthodontic alignment, which would be futile in cases of PFE.24,25
Management of PFE is particularly challenging. Treatment options are limited and complicated by the fact that diagnosis of the condition relies on a method of exclusion, where all other possible causative factors have been considered and eliminated rather than a positive finding. Options for management are summarized in Table 2 and range from most conservative to most invasive treatment options.
| Localized/Generalized | Treatment Options | Comments |
|---|---|---|
| Localized | 1. No active treatment | If there are no significant aesthetic or functional concerns acceptance of the position of the affected teeth is an option. |
| 2. Provision of a removable prosthesis over the affected teeth | This may be more predictable in achieving an acceptable occlusion. |
|
| 3. Coronal build-up/onlays of the affected teeth | This is an option with Type II PFE providing an acceptable occlusion can be achieved after vertical growth of the patient has ceased.27 Composite resin is the material of choice due to its adhesive property. Prosthetic management ensures occlusal stability and allows preservation of alveolar bone until after the pubertal growth spurt, where an osseointegrated implant can be considered but is limited to teeth which are mild-moderately infra-occluded with no occlusal interferences or over-eruption of opposing teeth. |
|
| 4. Surgical extractions of the affected teeth followed by prosthetic replacement. | Extensive bone loss may warrant a bone graft prior to implant placement |
|
| Exposure and bonding of teeth affected by failure of eruption attributed to PFE is not advised as treatment via active orthodontic forces has been suggested to lead to localized ankyloses29 | ||
| Generalized (multiple quadrants) | 1. Segmental osteotomy and a bone graft interposed between the segment and the basal alveolar bone | At best, an acceptable occlusion will be achieved and, at worst, the teeth will be moved into a more favourable position to aid prosthetic management. |
| 2. Distraction osteogenesis to correct an extreme posterior open bite | ||
Misdiagnosis and mismanagement of either condition can lead to:
Identifying patients with a known PTH1R gene mutation will aid better differentiation between MFE and PFE, based on their clinical presentation, to enable early treatment of cases with MFE and thereby give the clinician and the patient the confidence to pursue no treatment/more conservative management options in the case of PFE.
Moreover, dental clinicians who identify patients with PFE based on clinical suspicion and/or genetic confirmation should be aware that PTH1R variants have also been associated with other diseases listed in Table 3, which will warrant further investigations and management by relevant healthcare professionals.
| PTH1R Variants | Disease | Description |
|---|---|---|
| Complete loss of PTH1R function | Autosomal recessive Blomstrand chondrodysplasia32 | A rare skeletal dysplasia characterized by advanced endochondral bone maturation and premature ossification of all skeletal elements |
| Gain of function PTH1R mutations | Jansen type metaphyseal chondroplasia33 | Short-limb |
| Homozygous mutations | Autosomal recessive Eiken-Skeletal dysplasia34 | Multiple epiphyseal dysplasia and retarded ossification |
MFE and PFE are rare and similar in their presentation in the early stages. Differentiating between the two is paramount in making the correct diagnosis and managing the case successfully.