Abstract
In Part 2 of this article, we highlight the differences between the open and closed exposure techniques in the management of palatally displaced canines (PDCs), the mechanical principles of alignment and the management of ankylosis.
From Volume 15, Issue 4, October 2022 | Pages 175-180
In Part 2 of this article, we highlight the differences between the open and closed exposure techniques in the management of palatally displaced canines (PDCs), the mechanical principles of alignment and the management of ankylosis.

In this article, the differences between the open and closed exposure techniques are discussed, before focusing on the basic mechanical principles of alignment and the management of true ankylosis.
The evidence base in this area stems from two well-conducted, multicentre randomized clinical trials (RCTs) that investigated the effectiveness of open versus closed exposures for patients with PDCs. In one of these RCTs, Parkin et al reported that there were no differences between the techniques in terms of periodontal health, perceived discomfort, operating time, aesthetics and cost-effectiveness.1,2 Although there were also no statistically significant differences in the mean active alignment time of the two groups, the associated 95% confidence intervals were wider for the closed exposure group.3 This suggests that there may be less variability associated with the open technique, which may be reflective of the orthodontist's ability to visualize the direction of traction with this method.
In a more recent study, Björksved and colleagues also reported no differences in overall treatment times between the interventions; however, the research team did find statistically significant differences in relation to patient-reported discomfort (although this is unlikely to be clinically significant).4 A Cochrane systematic review in this field is currently being updated with the aim of increasing the power and precision of the data within this important research area.
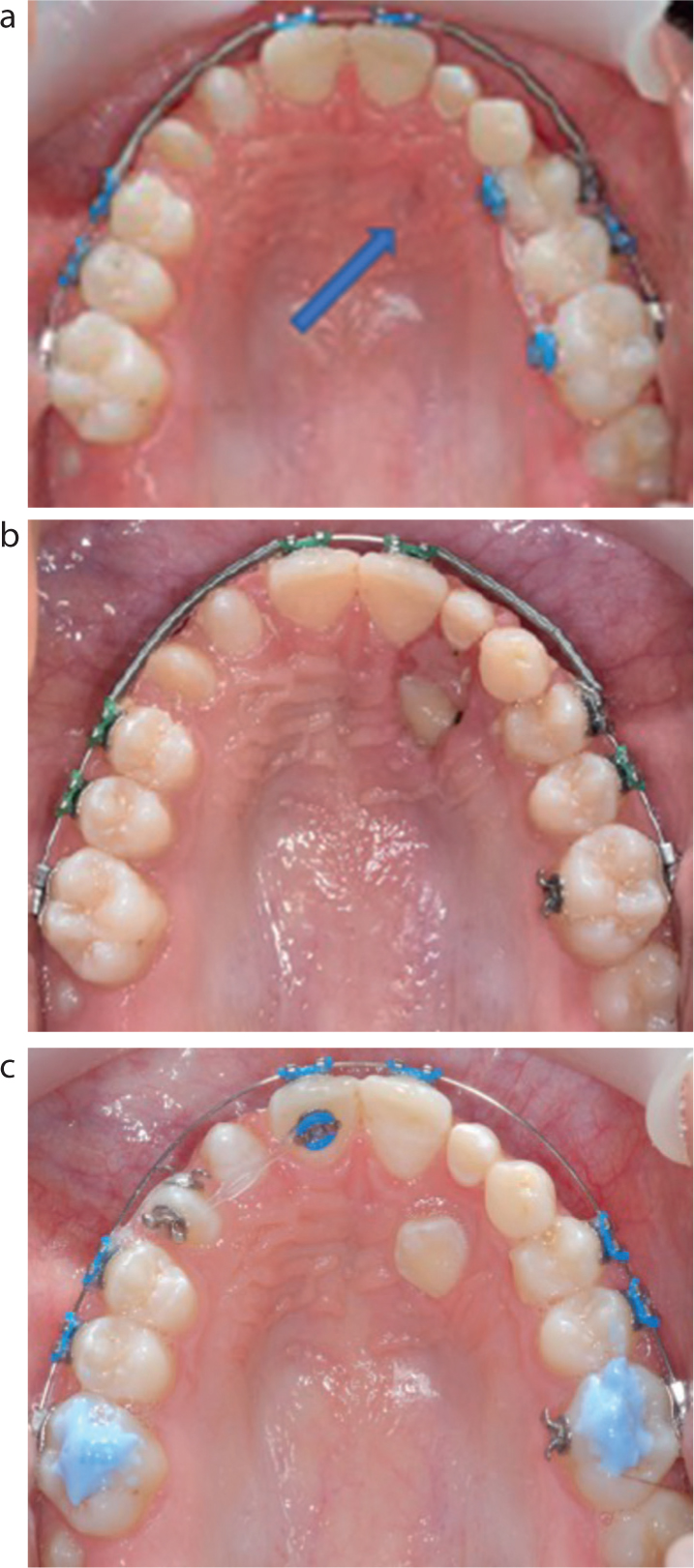
With this technique, palatal mucosa and bone overlying the canine are removed, with or without raising a mucoperiosteal flap. The exposed canine is then covered for approximately 10 days with either Coe-Pack (Figure 1), a cover plate or glass-ionomer cement, with the latter frequently used in Sweden despite limited evidence for its superiority.5 Following the procedure, the PDC is moved orthodontically above the mucosa.

An often-cited benefit of this option is that the PDC can erupt autonomously for up to 9 months before resorting to using any active forces (Figure 2).6 This may be particularly useful in the presence of short adjacent incisor roots. If necessary, other aspects of a patient's malocclusion can be addressed during this period of autonomous eruption (Figure 2). Although a rare occurrence, clinicians should be vigilant that PDCs exposed in this manner do not excessively over-erupt, particularly in the presence of an increased overbite, because this can complicate their alignment.

For spontaneous eruption to occur, sufficient bone must be removed around the crown at the time of surgery. Figure 3 demonstrates an inadequate open exposure, following which no autonomous eruption occurred. Occasionally, this can be salvaged by using retraction cord to maximize the surface area for bonding an attachment;7 however, if this is not possible, an additional surgical procedure may be required. The need for a sufficiently wide exposure must therefore be adequately communicated to surgical colleagues to minimize this unnecessary complication.
At the same time, orthodontists should ensure that their requests are realistic. This is particularly important when an open exposure is considered for a deeply impacted PDC, which is a technically difficult procedure.8 This extends to patients in the mixed dentition, as the vertical position of a high canine is likely to improve over time. In such instances, it is therefore usually sensible to delay surgery rather than complicate management unnecessarily.3
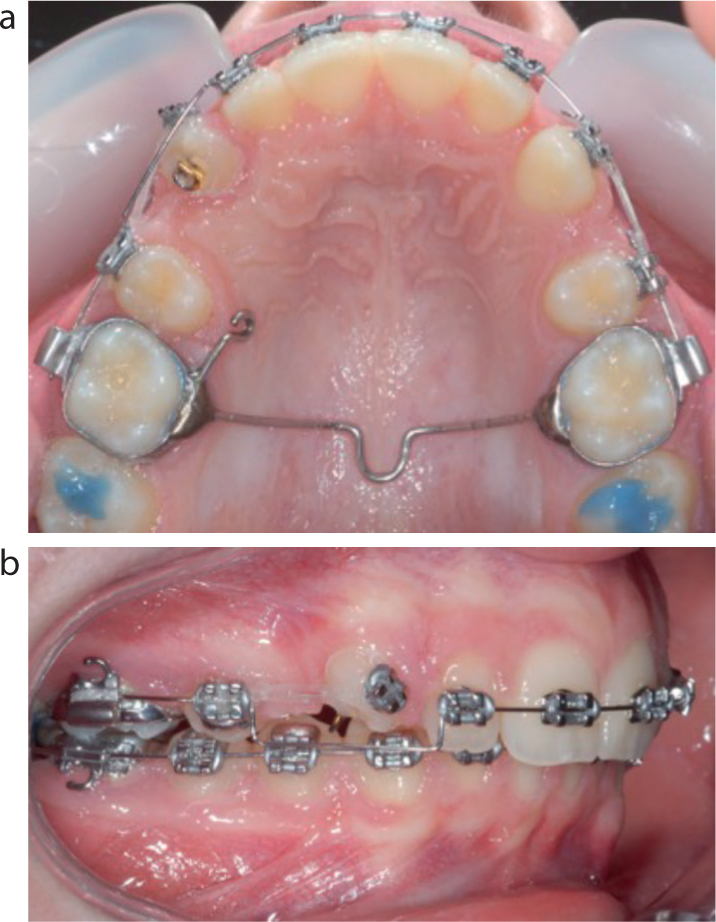
With a closed procedure, after raising a mucoperiosteal flap, identifying the PDC and removing sufficient bone, a gold chain is bonded to the tooth. This extends through the incision and is attached to either an adjacent tooth or to the upper archwire/mucosa with a suture.
With this technique, the PDC is aligned below the mucosa, making it harder to plan the direction of traction (Figure 4). Although a CBCT could be used to plan this more accurately, these are not routinely taken due to the increased radiation dosage and the cumulative impact of this in adolescents.9 A lack of direct visualization, and a resultant inappropriate force vector, may increase the risk of pseudo-ankylosis against the lateral incisor root or the buccal cortical plate.

With the closed technique, the orthodontist cannot see where the gold chain has been attached to the canine, which may be problematic unless this is documented during the operation or the chain is bonded by the orthodontist themselves. Ideally, the gold chain should be placed close to the tip on the buccal surface; however, due to difficulties with access and isolation, it is often bonded on the palatal aspect, resulting in varying degrees of rotation when the canine erupts (Figure 5). The subsequent requirement for derotation can lengthen treatment and potentially lead to gingival recession. The relative potential advantages and limitations of both techniques are shown in Table 1.
| Open exposure | Closed exposure | |
|---|---|---|
| Advantages | Promotes autonomous eruption,6 during which the primary canine can be left in situ to avoid a gap | Avoids the need for cover plate/Coe-Pack/GIC5 |
| Direct visualization enables planning of traction vector and optimal positioning of orthodontic attachment | No mucosal bunching | |
| Direct visualization of progress is possible | Gold chain is an easy initial application point for traction | |
| Disadvantages | Need for repeat procedure if exposure is suboptimal or OH is poor | Lack of direct visualization can lead to pseudo-ankylosis and larger variation in active alignment time3 |
| Cover plate/Coe-Pack/GIC required in immediate post-operative period | Difficulty placing gold chain in optimal position can lead to rotations | |
| Mucosal bunching during traction can lead to short clinical crowns | Debonding of gold chain, which may go unnoticed and require repeat procedure | |
| Technically difficult surgery for deeply impacted PDCs | Review of progress (often involving counting links of gold chain) is less obvious and may require radiographs | |
| Need to disengage occlusion during alignment | No spontaneous eruption so potentially higher extrusive forces required |
There are numerous techniques for applying orthodontic traction during alignment, the choice of which is generally dictated by the original position of the canine and the clinician's preference.10 However, due to the large positional variation of PDCs, mechanical flexibility is required to optimize treatment efficiency. Anchorage reinforcement, particularly in the transverse and vertical dimensions, should always be carefully considered at the start of treatment.
Mechanical eruption often involves moving the PDC distally (and therefore away from incisor roots) and occlusally in the first instance, before moving it buccally. This contrasts to a single-stage approach, in which the PDC is moved directly towards the line of the arch. The issue with the latter strategy is that the lateral incisor root can impede the PDC. With either approach, ideally the correct amount of space should be available before applying active traction towards the line of the arch. The various mechanical stages of alignment, which are often interlinked, will now be discussed.
If a PDC is close to the incisal roots, a gold chain offers an easy application point for immediate distal movement. With an open exposure, particularly if there has been insufficient autonomous eruption, or if only the palatal aspect is visible, achieving distal movement can initially be more awkward. In this case, the PDC can either be vertically erupted first, or an attachment can be bonded to pull the tooth distally, away from the incisors.
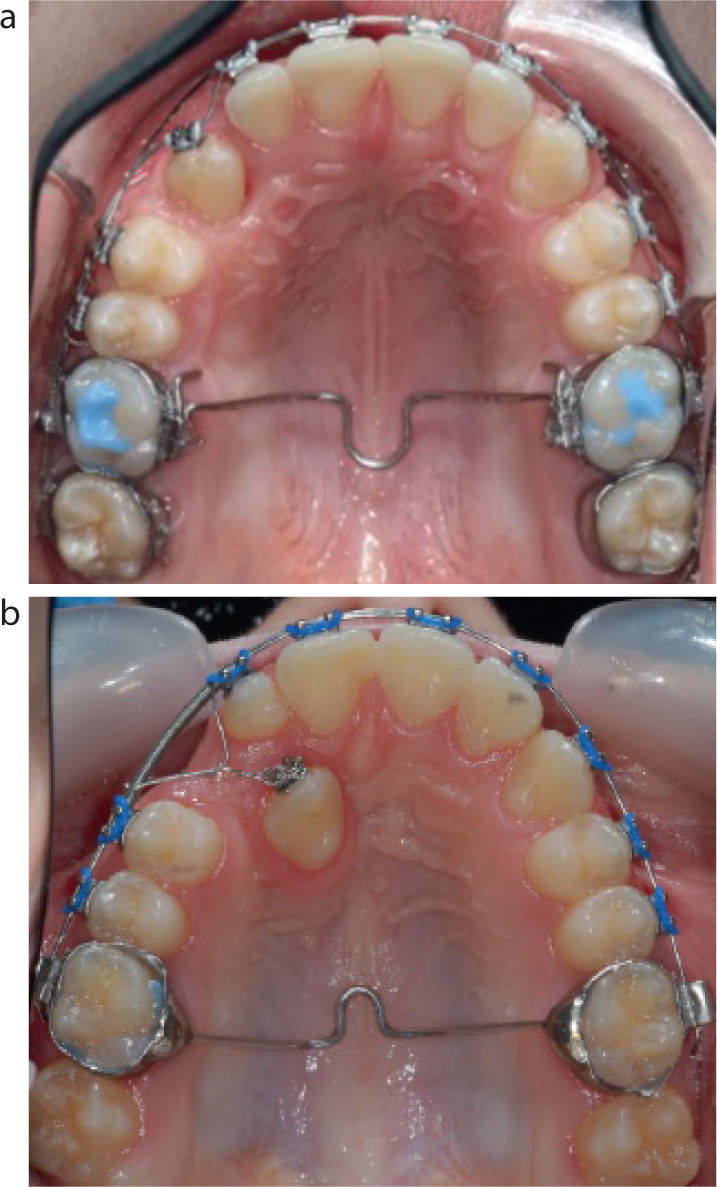
Distal movement can be commenced using a transpalatal arch (TPA) with soldered hooks, spurs or whip springs, as well as palatal orthodontic attachments (Figure 7) and palatally positioned temporary anchorage devices (TADs). If the latter are planned then it is worthwhile considering their placement at the time of the surgical exposure, providing this will not interfere with the desired flap design.


Vertical mechanical eruption is almost always required with the closed technique. Ballista springs, which are flexible loops usually bent up in ‘off the reel’ stainless steel (Figure 7), can be used for this purpose.11 Care must be taken to ensure that these are not overactivated, as this can reduce the bony support for the PDC, and progress should be monitored vigilantly. Vertical eruption with this technique may also be required where limited autonomous eruption has occurred with the open technique.
For patients with short maxillary incisor roots, it is usually desirable to limit the forces that these teeth are subjected to. There are several options to effect vertical movement in such situations, including fishing rod mechanics using a TMA buccal auxiliary archwire, which requires double-tubed molar bands and potentially vertical anchorage reinforcement.
TADs, inserted either buccally in the mandibular arch, or in the anterior palate can also be used for this purpose.12 The potential advantages of increased TAD stability with using the anterior palate as an insertion site13 must be weighed up against patient comfort from having to use fairly large laboratory-constructed appliances to ensure an appropriate force vector for canine alignment. Magnets can also be used for vertical eruption, but their use has been largely superseded.14
Delaying the bonding of adjacent short-rooted lateral incisors until a PDC is near alignment is another worthwhile consideration. As well as limiting root resorption, this should minimize any vertical bone loss around the distal aspect of the lateral incisor.

Ideally, an attachment should be bonded as close as possible to the mid-buccal surface of the PDC before active traction towards the arch takes place. In the presence of an increased overbite, or an over-erupted opposing tooth, the occlusion will need to be temporarily disengaged, particularly if an open exposure has been carried out.
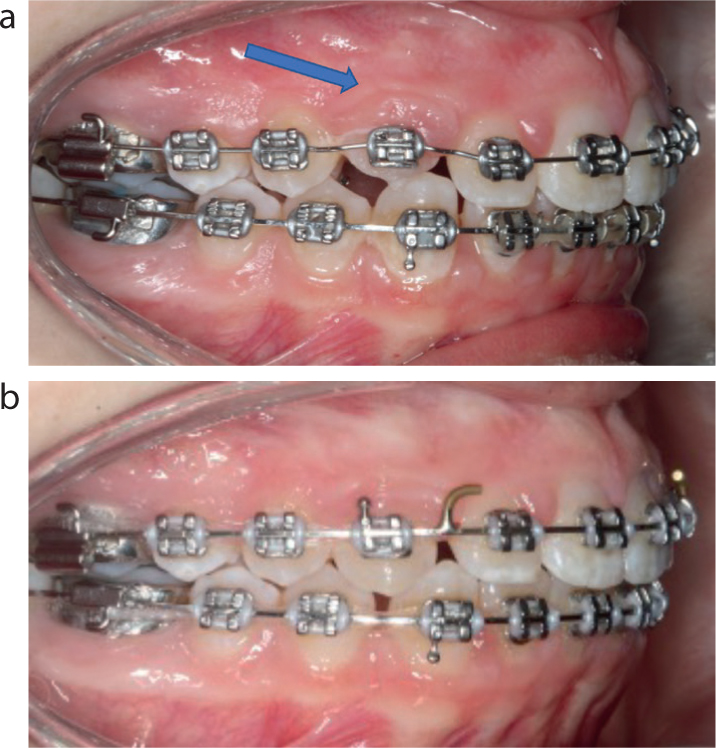
With an open technique, if the tooth has not erupted sufficiently before this traction is applied, then gingival bunching can occur (Figure 10). If this impedes movement then the mucosal cuff can be excised; however, care is needed due to the proximity of the anterior palatine artery.11 It is therefore preferable to use smaller attachments and promote excellent oral hygiene to prevent bunching from occurring in the first place.
The piggyback technique, which uses a rigid base archwire to provide vertical and transverse anchorage, while a nickel titanium archwire brings the malpositioned tooth into the line of the arch,15 can be used to effect both vertical and transverse movement. If the PDC is severely medially displaced, the piggyback archwire can be partially activated with a stainless-steel ligature (Figure 8). Where indicated, offsets can be placed in the base archwire to maintain space and increase the range of possible tooth movement. If elastomeric traction is used as an alternative, then push-coil can be used to facilitate directional control.
Other options include the sling-shot technique, either on its own or concurrently with a piggyback, and TPAs with an active arm to push the PDC towards the line of the arch.16 TADs can also be placed vertically in the alveolus and used for direct anchorage (Figure 9). This approach minimizes forces on adjacent incisors and is therefore advantageous if the canine needs to be moved a considerable distance, particularly in the presence of short incisor roots.
Once the tooth has been moved across the occlusion, a canine bracket (or an alternative with more buccal root torque) will need to be placed in the optimal position to enable the root to be torqued buccally. In the presence of bunching, some extrusion may be required to enable optimal bracket repositioning at a subsequent visit (Figure 10).
As PDCs are aligned using a round archwire, they often require buccal root torque (BRT) to improve both their appearance and stability, with the duration of this stage related to the initial palatal displacement of the root (Figure 11). Adequate BRT is usually achieved by spending sufficient time in a full-sized archwire but can be facilitated by third order archwire bends and torqueing auxiliaries.
There is minimal evidence to suggest the superiority of a particular retention regimen for PDCs.17 However, having to derotate a PDC by a significant amount, often towards the end of treatment, could plausibly lead to a higher relapse potential due to the action of the trans-septal fibres18 and may warrant the use of bonded retention.
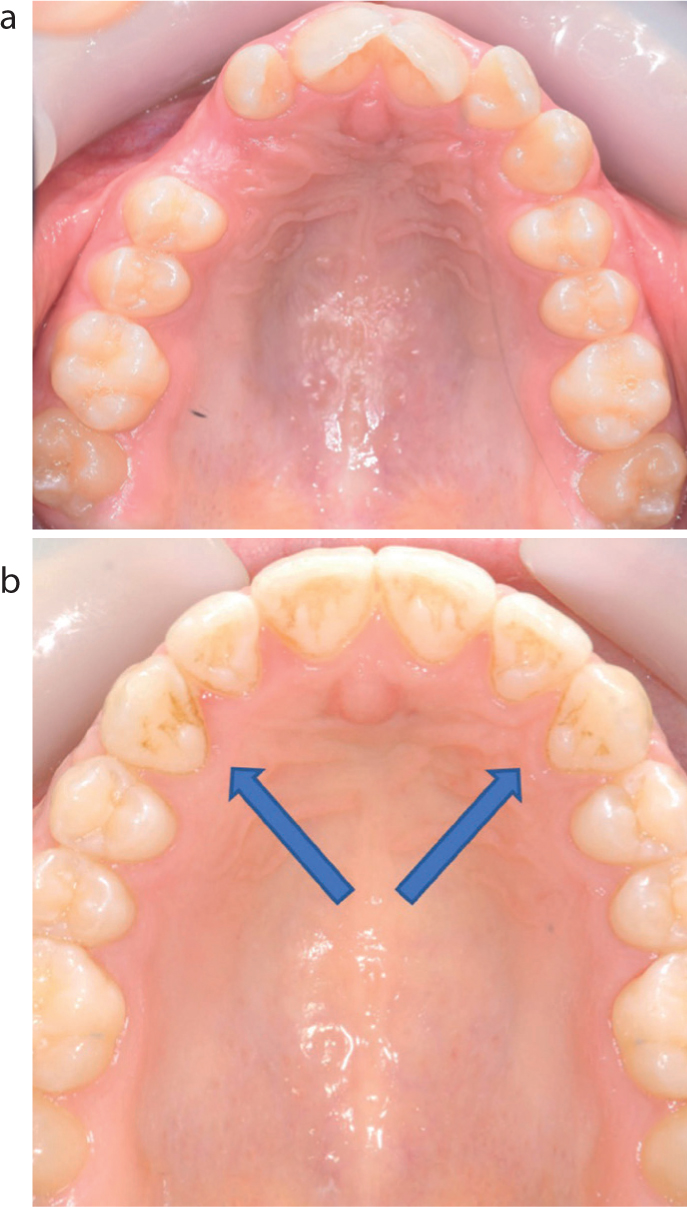
Clinicians should be mindful of signs of true ankylosis, particularly when attempting alignment in older patients. This may include relative intrusion of adjacent teeth, with canting of the occlusal plane, the development of a vertical bony defect and loss of arch form (Figure 12). If true ankylosis and resultant anchorage loss occurs, active traction should be stopped to allow the arch form to recover while mechanics are re-evaluated. Further treatment options are likely to depend on the amount of time the patient has already been in treatment and the position of the PDC at that point (Table 2).

| Treatment | Advantages | Disadvantages |
|---|---|---|
| Accept position +/- restorative build-up | Suitable if low smile line and almost aligned | Sub-optimal aesthetics |
| Increased vertical crown height | ||
| Continue orthodontic traction (intermaxillary elastics; URA with buccal arm; TADs) | FAs will already be in situ | Canting of occlusal plane (elastics) |
| Excellent compliance needed (RAs) | ||
| Difficult to control vector with TADs if used for direct anchorage | ||
| Auto-transplantation (Figure 13) | Maintenance of tooth | Technique-sensitive surgery |
| RCT required as root apex likely to be mature | ||
| Adequate space is needed | ||
| Block segmental osteotomy with repositioning/distraction osteogenesis | Maintenance of tooth | Requires technically difficult surgery |
| Difficult to optimise distraction vector | ||
| Extraction and space closure | No requirement for prosthesis | Bone loss following extraction can impede space closure |
| Prolongs time in FAs | ||
| Extraction and prosthetic replacement with implant/resin-bonded bridge (RBB) | Avoids prolonging FA treatment | Bone grafting required for implants if bony defect present |
| Cost and maintenance of prosthesis |

The treatment of PDCs can be challenging for both patients and orthodontists. The wide positional variation in their presentation, as well as the potential for co-existing dental and occlusal anomalies, means that there is no one-size-fits-all approach to their management. The one uniting factor is that clinical success is related to operator flexibility with different treatment mechanics, often in the same patient.