References
Distraction Osteogenesis Part 1: History and Uses in the Craniofacial Region
From Volume 11, Issue 1, January 2018 | Pages 14-20
Article

History of distraction osteogenesis
Distraction osteogenesis (DO) originated as a method to repair skeletal deformities and large, non-healing, segmental bone defects resulting from injuries suffered by Russian soldiers during World War II. The method, which increases the length of bones by causing new bone to form between two surgically separated segments of bone, was discovered inadvertently by a non-surgically trained general practitioner, Gavril Ilizarov, in a small town in Siberia. Subsequently, Professor Ilizarov became a renowned orthopaedic leader due to the revolutionary advancements in bone management arising from DO. However, the discovery of DO in the mid-20th Century did not initially reach Western Europe due to delays caused by the Cold War.1
Distraction osteogenesis in the craniofacial region
Craniofacial distraction was first reported in 1973 by Snyder and co-workers, who demonstrated resection and subsequent reconstruction of a section of canine mandible using distraction with an extra-oral fixation device.2 Translation of the technique to human craniofacial structures came some years later, when successful mandibular distraction was described in four children with congenital mandibular hypoplasia in 1992.3 A report of more extensive three-dimensional movement using miniaturized distraction devices in a 4-month-old boy with left-sided craniofacial microsomia in 1995 emphasized wider potential applications for the technique.4 In the 20 years since, numerous reports of craniofacial distraction osteogenesis have been published.
The biological basis of distraction osteogenesis
Bone is a unique and highly specialized tissue, rigid and hard but capable of adaptation and regeneration. DO relies on the bone's capacity to repair and remodel following damage, resulting in new bone formation with preservation of strength. DO creates new bone through the same process used for fracture repair. Initially, the bone is sectioned surgically and a latency period is allowed for development of a callus. Migration of inflammatory cells and haematoma formation occurs in the site of the bony cut, followed by formation of a fibrovascular bridge from fibroblasts and newly formed blood vessels, organized in the direction of distraction. The activation period follows this, with stretching of the callus in a gradual, controlled, incremental manner using a distraction device. Separation of the sections generates tension that stimulates new bone formation parallel to the vector of traction. Once sufficient lengthening has been achieved, the activation ceases and a consolidation period is allowed whilst the callus calcifies prior to removal of the distraction device (Figure 1).

Histologically, DO replicates intramembranous ossification with four stages:5,6,7
The stages overlap throughout the lengthening process with a central zone of primarily fibrous tissue and increasingly mature bone adjacent to the bony edges. Within 8 months of active distraction, the newly formed bone achieves 90% of the normal bony architecture and is believed to be able to withstand normal functional loads.7
Importantly, and unlike bone grafting techniques where bone is transferred from one site to another, DO creates new bone while simultaneously expanding the soft tissues at the same rate. Alongside this, tension in the surrounding soft tissues initiates adaptive changes known as distraction histogenesis. Distraction histogenesis occurs in skin, fascia, blood vessels, nerves, muscle, ligament and cartilage.8
Advantages and disadvantages of distraction osteogenesis
The incremental bone lengthening and associated gradual soft tissue stretch achieved through DO has a number of advantages when compared to conventional orthognathic surgery:
As with all techniques, there are a number of potential disadvantages to be considered:
Application of distraction osteogenesis
Distraction osteogenesis originated as a method for encouraging healing of bone infections and uniting fractures. Today, the main application of DO in craniofacial structures is the management of bony defects arising as a result of developmental anomalies, trauma or pathology9 (Table 1).
| Aetiology of Deformity | Presentation | |
|---|---|---|
| Developmental | Condylar hypoplasia | Reduced ramus height with or without TMJ functional limitations. May be uni- or bilateral |
| Mandibular hypoplasia |
Reduced mandibular size in all planes |
|
| Condylar hyperplasia | Facial asymmetry with chin point deviation to contralateral side | |
| Maxillary hypoplasia |
Retrognathic midface with relative protrusion of the mandible resulting in a Class III skeletal pattern |
|
| Hemifacial microsomia20 | Variable severity including skeletal facial asymmetry associated with aplasia/hypoplasia of the mandibular ramus and condyle and reduction in size or flattening of the facial bones |
|
| Treacher Collins syndrome20 | Variable severity resulting in underdevelopment of the supraorbital and zygomatic bones and mandible |
|
| Syndromic craniosynostosis including Crouzon's, Apert's and Pfeiffer syndrome17 | Midfacial retrusion, shallow orbits, exorbitism, malocclusion, obstructive sleep apnoea and facial imbalance | |
| Traumatic | Trauma to condyle during growth21 | Disturbed mandibular growth or temporomandibular joint ankylosis resulting in mandibular asymmetry |
| Facial trauma during growth22 | Abnormal growth as a result of damage to growth centres, soft tissue injury and subsequent scarring, iatrogenic damage from soft tissue/periosteal stripping or fixation methods, or fracture malposition |
|
| Pathological | Non-malignant but locally aggressive eg ameloblastoma, odontogenic keratocyst | Large areas of bony deficit following removal of mass or resection |
| Malignant lesions such as osteosarcoma and bony metastases | ||
| Infective | Otitis media | Abnormal growth or TMJ ankylosis resulting in mandibular asymmetry |
| Autoimmune | Juvenile idiopathic arthritis23 | Abnormal growth or TMJ ankylosis resulting in mandibular asymmetry |
DO aims to normalize the craniofacial structure to optimize growth and development in growing patients, and correct anomalies in shape, size or structure to improve function and aesthetics.8 Mandibular hypoplasia or retrognathia associated with abnormal anatomy can lead to respiratory problems due to soft tissue obstruction of the upper airway (obstructive sleep apnoea). Mandibular distraction can reduce the need for a tracheostomy in younger children and improve obstructive symptoms in older children.10
Theoretically, DO can be used to expand any bone in all three planes, allowing change in the shape and form of bones.8 However, consideration should be given to a number of anatomical features when planning and undertaking DO.11
Unilateral distraction can be undertaken in cases with asymmetry as a result of a deficit or hypertrophy affecting only one side. Restrictions in unilateral lengthening due to the articulation of the bones mean a relieving bony cut is often required on the contralateral side to enable activation of the distraction device. In cases with a bilateral bony deficit, distraction can be undertaken on both sides simultaneously through placement of bilateral distraction devices.
Mandibular distraction
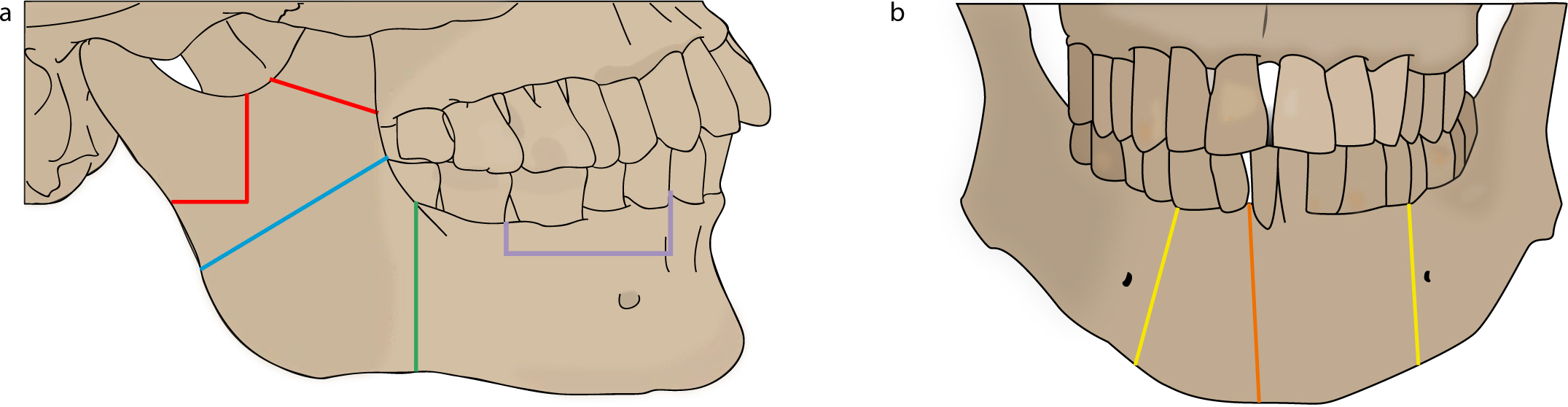
The direction of mandibular distraction will depend on the direction and site of the osteotomy cut and the vector of the distractor. The possible applications of DO in the mandible are illustrated in Figure 2. Vertical lengthening can be achieved by transporting the condyle up into the glenoid fossa or by increasing the ramus length. Horizontal lengthening is achieved through osteotomy and distraction along the body of the mandible. An oblique osteotomy at the angle of the mandible with placement of a multidirectional distractor facilitates lengthening in both a vertical and horizontal plane.12 Transverse expansion is less commonly reported but can be accomplished by a vertical osteotomy in the symphyseal region and activation of a tooth-borne distractor.13
More recently, localized distraction in the alveolus has been proposed as an alternative to block grafts for vertical augmentation of the alveolar ridge. Atrophy of the alveolar ridge is a common sequelae of tooth loss as a result of trauma or pathology and vertical augmentation is recognized as being challenging. Distraction osteogenesis of edentulous segments of the alveolus can facilitate placement of implants for reconstruction by increasing the width and height of bone.14 Vertical alveolar distraction has been reported in mandibular reconstruction following a large odontogenic keratocyst.15
Maxillary distraction osteogenesis
The most common application for maxillary DO is in the management of maxillary hypoplasia for cleft lip and palate patients. Maxillary advancement is achieved through a Le Fort I separation and placement of a distractor to achieve a horizontal vector of expansion.11 A more familiar distraction osteogenesis procedure for orthodontists is Surgical Assisted Rapid Palatal Expansion (SARPE), which is routinely used alone or as an adjunct to conventional orthognathic surgery.16 As with mandibular applications, alveolar height can be developed through distraction of a block of alveolar bone (Figure 3).

Midface and cranial distraction osteogenesis
Distraction osteogenesis has gained popularity for advancement of the midface using a Le Fort II or III procedure as greater movements are possible and pleasing repositioning of the lips, cheeks and eyelids often results. Advancement of the maxilla and nasal complex will occur with a Le Fort II approach, and is therefore preferred for those with an acceptable position of the zygomatic complex and orbits. A Le Fort III approach will result in advancement of the whole zygomaxillary complex and is commonly reported for management of Apert's and Crouzon's syndrome and to reduce relative globe proptosis, preventing potential ophthalmic complications such as amblyopia, corneal exposure with subsequent exposure keratitis, corneal ulceration, cataracts and vision loss. In addition, expansion of the oropharynx and nasopharynx can address respiratory problems and facilitate removal of the tracheostomy. For midface retrusion in combination with forehead retrusion, the Le Fort III can be converted into a monobloc procedure or distraction osteogenesis can be staged.17
The versatility of DO in the midface is illustrated by numerous reports of its use, including distraction of the zygoma and orbit, nasal bone distraction in hypertelorism and distraction of scarred soft tissue before secondary bone grafting.9 Cranial distraction can be undertaken in isolation or in conjunction with midfacial distraction procedures.
Transport distraction osteogenesis
Distraction osteogenesis can be described in terms of the number of foci at which osteogenesis occurs. The majority of procedures in the craniofacial region are monofocal, aiming to increase bone length. An alternative type of DO used for reconstruction of a significant segmental bone defect is a bifocal method called transport distraction. In this technique, bone is created by gradually moving a disc of bone across a defect, leading to bone formation behind the disc (Figure 4). Trifocal distraction is similar but discs are transported from both ends to meet in the middle, with the aim of reducing the required distraction time. Transport distraction can be used for condylar reconstruction and as an alternative to bone grafts, allogenic materials and vascularized free flaps in cases with segmental loss of bone as a result of severe trauma or tumour resection.18,19

Summary
Distraction osteogenesis is a versatile technique that can be used to treat a number of bony defects in the craniofacial region. The capacity to create new bone and simultaneously encourage soft tissue adaptation provides opportunities for managing conditions that are less amenable to conventional orthognathic surgery techniques. In the second part of this review we will discuss planning and undertaking distraction osteogenesis.
