References
Demonstrating the benefit of self-ligating brackets in the management of severe dental crowding on a non–extraction basis
From Volume 10, Issue 4, October 2017 | Pages 151-156
Article
The first self-ligating bracket (SLB) was described by Stolzenberg in the 1930s1 and introduced as the Russell lock edgewise attachment. The concept of the SLB has not changed much since that introduction. However, the use of the design has become much more mainstream in the last three decades, so much so that the success of the Damon type bracket is almost synonymous with a form of treatment. Due to this growing demand from both the orthodontist and the patient, many new bracket types have been described. These are all based around having a spring clip which ‘locks’ the archwire in position, ie excluding the use of elastics or wire ligatures. These brackets can further be subdivided into their ‘active’ or ‘passive’ variants. The active form has a spring clip which presses against the archwire and in the passive form the clip does not come into contact with the archwire.
The benefits of SLBs have been proposed and include shorter treatment times, treatment on a non-extraction basis, less discomfort and better oral hygiene.2 However, none of these has been substantiated by randomized clinical trials. This case report demonstrates a clinical scenario in which it was desirable to avoid dental extractions, because of skeletal presentation; an interesting point was that the upper right canine was so buccally impacted that, had conventional ligation been used, it is likely that extraction in one or both arches would have been necessary. Self-ligating brackets were selected in order to capitalize on their low friction properties, in the hope that this would facilitate the easier opening of space to accommodate permanent teeth on a non-extraction basis. This has been successful, therefore we propose that the primary benefit of SLBs is their ability to open space to accommodate impacted teeth on a non-extraction basis. Self-ligating bracket systems help to achieve an ideal treatment plan which would otherwise be difficult to execute using conventional ligation bracket systems.
The debate of extraction versus non-extraction orthodontics is as alive as it was when it was first initiated over 100 years ago. Whilst it is correct to extract teeth in appropriate cases, such as those with moderate to severe crowding, there are instances when dental extractions are undesirable. For example, in Class III cases, non-extraction treated patient groups have been shown to have improved mandibular positions accompanied with an improvement in facial convexity.3 For paediatric and adolescent patients, extractions can be difficult and may result in bad experiences which have been shown to affect future access to dental care psychologically.4,5 Furthermore, for a small number of patients it can avoid the use of general anaesthesia and the potential risks associated with this form of anaesthetic.
Case report
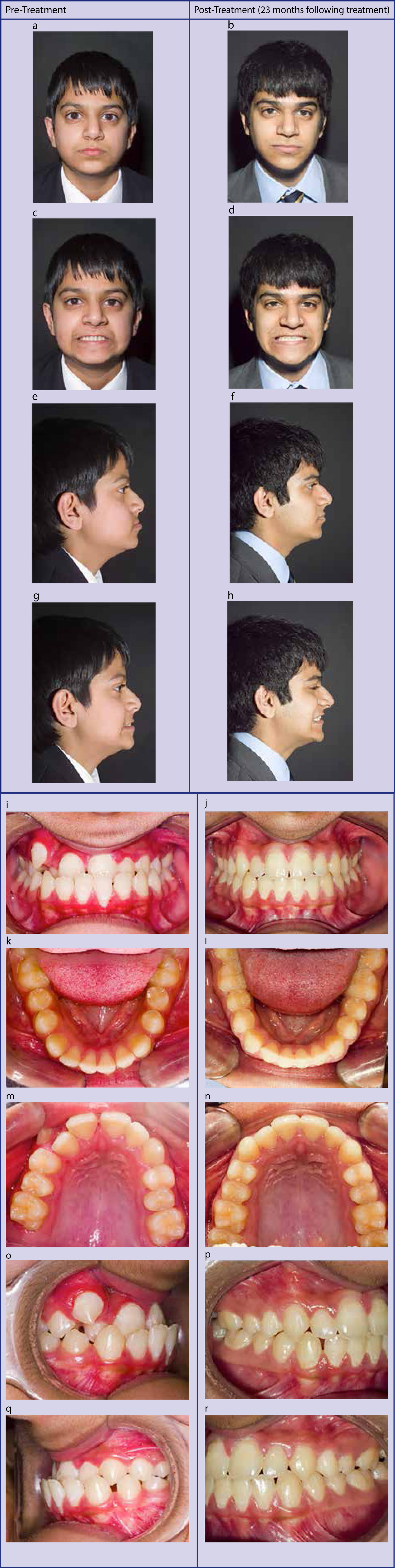
A 10-year-old male, of South-East Asian decent, was referred from his primary care orthodontist to the hospital orthodontic department for a second opinion and help with treatment planning. The patient's main presenting complaint was the fact that he was ‘unable to eat properly’. There was no relevant medical history.
The patient presented with a mild Class III skeletal pattern with reduced FMPA and reduced anterior lower face height. There was no mandibular displacement during closure. No facial asymmetry was noted. The lower lip was everted.
The patient presented in the mixed dentition phase with a well aligned and spaced lower arch. He had bimaxillary proclination, with a buccally impacted upper right canine. Consequently, there was an upper midline shift to the right. He had a reverse overjet with a normal overbite. The incisor relationship was Class III and the molar relationship was Class I bilaterally. Additionally, he had a bilateral crossbite tendency. The patient presented with a very unusual problem; a severely crowded Class III malocclusion with significant upper centreline shift, on a low angle skeletal 3 base with bimaxillary proclination of the upper and lower incisors.
A radiograph (Figure 1) confirmed the presence of all permanent teeth except for the third molars at this stage. The lateral cephalograph confirmed a mild skeletal Class III discrepancy with proclination of the lower incisors, demonstrating scope for retroclination to correct his reverse overjet (Figure 2, Table 1).
| Actual | Mean | |
|---|---|---|
| SKELETAL | ||
| SNA° | 81.5 | 81.5 |
| SNB° | 83.0 | 78.0 |
| ANB° | -1.5 | 3.0 |
| SN/MxP° | 9.0 | 7.5 |
| MxP/MnP° | 16.5 | 27.0 |
| LAFH/TAFH % | 52.5 | 56.0 |
| TEETH | ||
| Overjet mm | -4.5 | 3.5 |
| Overbite mm | 4.5 | 4.0 |
| UI/MxP° | 21.5 | 109.0 |
| LI/MnP° | 107.5 | 92.0 |
| LI-Apo mm | 10.0 | 1.0 |


Treatment
Rapid maxillary expansion was used to expand the maxillary arch. Posterior acrylic bite capping attached to the expander was used to open the bite, to allow the lower incisors to retrocline, achieved with Class III traction applied to a lower fixed appliance. Once this phase had been completed the upper arch was bonded with self-ligating brackets (Smart Clip). Space was created to bring the buccally impacted canine into the line of the arch and to correct the upper dental midline.
During the treatment phase, the patient's oral hygiene became poor and he was urgently referred to a general dental practitioner, which resulted in vast improvement. However, his orthodontic treatment was curtailed slightly as a result.
The total active treatment time was 23 months.
Clinical photographs before and after treatment were taken (Figure 3 a–r).
Discussion
Orthodontic patients often present with a multitude of dental disturbances which make treatment both challenging and rewarding for the practitioner. Kotsomitis et al report that, from a sample base of 202 orthodontic patients (101 twin pairs), ectopic eruption was observed at a rate of 29.7%.6 Teeth which have a high prevalence of ectopic eruption in order of frequency are: mandibular third molars, maxillary canines, maxillary first permanent molars, mandibular canines, mandibular second molars and maxillary lateral incisors.7 Aligning these ectopic teeth into the arch requires space. Often space is created through the extraction of units. However, this case report demonstrates the creation of space using SLB systems.
Whilst it may have been possible to open space with conventional brackets, we believe this to be unlikely or much more difficult.
How is space opened successfully with self-ligating brackets? One postulation would be that SLBs have lower frictional properties when compared to their conventional counter-parts. To increase efficiency of tooth movement over time, the frictional force component should be reduced. For this very reason there has been a substantial amount of scientific research in the last five decades with an aim to reduce this friction. Different forms of bracket design and wire materials have been investigated and described in western literature.8,9 Friction can be subdivided into static and kinetic components, of which the static form is of more importance during orthodontics.10 An ex-vivo study comparing static friction associated with SLBs and conventional brackets (CBs) demonstrated lower levels associated with SLBs for zero angulation. As angulation increased, so did the static resistance. Pizzoni et al11 and Thomas et al12 demonstrate SLBs providing less frictional resistance when compared to CBs. Pandis et al13 describe a study comparing force levels needed for certain tooth movement by CBs and SLBs. They reported a reduction in force required by SLBs to encounter the same displacement when compared to CBs. This reduction is more notable for correction in the bucco-lingual direction and less so in the intrusion-extrusion movement. Many studies corroborate this reduction in friction when using SLBs compared to CBs, some of which reach high clinical significance.12,14,15 Thorstenson and Kusy15,16 describe how, at all differing degrees of tip, a certain SLB bracket produced significantly less resistance to sliding. There was a difference of 60 g between CB and SLB communicated at an angulation of six degrees for a 0.018” x 0.025” archwire. It would be naїve to assume that all SLB bracket types lead to decreased frictional forces which are clinically significant. SLBs can have frictional forces which are variable and can reach high magnitudes.
In our case report, we show the movement of severely malpositioned teeth using SLB systems. Bacetti et al17 present an interesting experimental model where they demonstrate orthodontic forces released by SLBs compared to CBs during alignment of apically or malpositioned teeth. In this study, they reveal that, for buccal or apical misalignments of greater than 6.0 mm, the SLBS generate a force significantly greater than when compared to CBs. This provides potential support for the use of SLBs in the management of moderately to severely misaligned teeth.
The many claims of SLBS, notably shorter treatment times, reduction in discomfort, improved oral hygiene, greater aesthetics, have been shown to be inconclusive when comparing different research studies.18 As clinicians, our primary aim should be to achieve the best possible treatment outcome for our patients.
We propose the primary benefit of self-ligating brackets is that they can help to achieve this in cases where extractions are preferably avoided, but the limited amount of space at presentation makes this challenging.
Conclusions
In selective cases, with severely ectopic teeth together with a lack of space in the arch, SLBs can be utilized to achieve arch alignment which conventionally would require extraction of teeth. The clinical significance must be weighed up by the orthodontist when managing his/her patient on an individual basis. Therefore, it is important that the orthodontic practitioner is aware of this treatment option when planning cases requiring large movements of units into crowded arches.
