References
Article

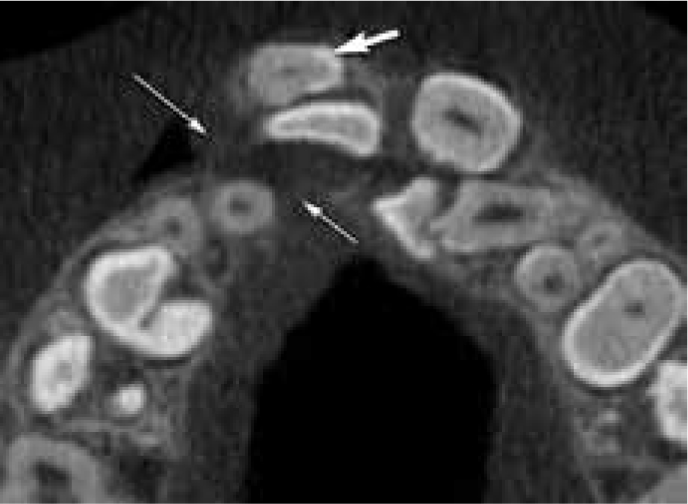
Orthodontic diagnosis and treatment planning has been carried out successfully using 2D dimensional imaging for many years. Cone beam computed tomography (CBCT) provides the clinician with 3D information which, in selected cases, may be beneficial in the management of difficult and complex cases.
The aim of this article is to outline the use of CBCT in orthodontic management, focusing on the current selection criteria (justification), the methods of dose reduction (optimization), as well as outlining the current guidance regarding reporting (evaluation) of CBCT scans.
Overview of CBCT Imaging
The patient is generally either sitting or standing in the unit and positioned using light beam markers. Once correctly positioned, the patient is then immobilized to reduce movement artefact. The appropriate imaging parameters and volume size or field of view (FoV) are selected. The cone-shaped X-ray beam and the detector rotate around the patient, acquiring frames of data throughout the rotation. Typically, several hundred frames are acquired, and from this a 3D data set is reconstructed. Secondary reconstruction into axial, coronal and sagittal planes can then be made.
The spatial resolution (the ability to distinguish two structures close together) of CBCT images is generally lower than traditional 2D imaging, but higher than the alternative medical grade computed tomography imaging. The contrast resolution (the ability to distinguish adjacent structures that have only small differences in density) is poor compared to medical computed tomography. This means that, although soft tissue boundaries with air can be seen allowing airway space assessment, CBCT is unable to differentiate the various soft tissues from one another. CBCT can only be used to assess hard tissues in detail.
Selection criteria for CBCT
In 2012, The European Commission published Evidence-Based Guidelines on Cone Beam CT for Dental and Maxillofacial Radiology.1 This work was carried out by the SEDENTEXCT group and provided comprehensive guidance on several aspects of CBCT imaging, including justification and optimization of CBCT exposures. General and specialty specific evidence base guidelines were produced for all areas of dentistry, including orthodontics.
Each guideline was assigned a grade, depending on the levels of evidence available. None of the orthodontic guidelines had high levels of evidence to support the statements and, in most cases, were based on ‘good practice’. The guidelines applicable to orthodontics are reproduced from the guidance notes in Table 1.
| Clinical Indication | Guideline |
|---|---|
| Unerupted tooth localization | For the localized assessment of an impacted tooth (including consideration of resorption of an adjacent tooth) where the current imaging method of choice is Multislice CT (MSCT), CBCT may be preferred because of reduced radiation dose |
| External resorption in relation to un-erupted teeth | CBCT may be indicated for the localized assessment of an impacted tooth (including consideration of resorption of an adjacent tooth) where the current imaging method of choice is conventional dental radiography and when the information cannot be obtained adequately by lower dose conventional (traditional) radiography |
| Cleft palate | Where the current imaging method of choice for the assessment of cleft palate is MSCT, CBCT may be preferred if radiation dose is lower. The smallest volume size compatible with the situation should be selected because of reduced radiation dose |
| Temporary orthodontic anchorage using ‘mini-implants’ | CBCT is not normally indicated for planning the placement of temporary anchorage devices in orthodontics |
| Orthognathic treatment planning | For complex cases of skeletal abnormality, particularly those requiring combined orthodontic/surgical management, large volume CBCT may be justified in planning the definitive procedure, particularly where MSCT is the current imaging method of choice |
| General points |
|
In 2015, the 4th edition of Guidelines for the Clinical Use of Radiographs in Clinical Orthodontics was published.2 The section on CBCT has been updated since the previous edition. The recommendations made are in line with those published by the European Commission in 2012. Large field of view scans could not be recommended in Orthodontics. A summary of the indications for small field of view CBCT scans is shown in Table 2.
|
|



Dose optimization
The effective doses from CBCT are generally higher than conventional dental radiography. The effective dose from a panoramic radiograph is in the order 2.7–38 µSv and the dose from a periapical 0.3–21.6 µSv.3 The dose arising from CBCT investigations varies greatly and a recent meta-analysis of published data for nine CBCT units showed the dose varied between 5–1073 µSv.4 The lifetime attributable cancer risk expressed as a probability to develop radiation-induced cancer has been calculated for 2 CBCT units as 6 per million.5 In addition, many orthodontic patients are children and the cancer risk is 2–3 times higher than for adults.6 It is therefore particularly important that all doses are fully optimized for children. Dose optimization can be achieved in the following ways.
Field of View (FoV)
The field of view has great influence on the effective dose. The field of view can be categorized into small (volume ≤10 cm in height), medium (volume 10–15 cm in height) and large (volume >15 cm in height). The average dose for the nine units studied in the meta-analysis by Ludlow et al was 84 µSv for small FoV, 177 µSv for medium FoV and 212 µSv for large FoV.4 It is important that the volume size selected is appropriate to the clinical question being posed. The smallest volumes must always be selected. Many clinical questions in orthodontics can be answered by using volumes of 4 cm3.
Exposure factors, arc of rotation and voxel size
Several units now allow the operator to reduce the exposure factors (time of exposure, current (mA), and kilovoltage (kV)). It has been shown that significant dose reductions can be obtained by reducing the exposure factors without any detrimental effect to accuracy of measurements.7,8 In one clinical study, it was shown that the exposure factors could be reduced to 1/8th of the manufacturers recommended exposure settings.9 This did produce noisier images but the studies could still be used, particularly if 3D virtual models were not required.
Some units offer the ability of being able to reduce the arc of rotation of the x-ray source and detector around the patient. Essentially, this reduces the number of frames that are acquired during the scan. Switching from a 360-degree rotation to a 180-degree rotation reduces the dose by around 50%.10 Scans using this mode still have good subjective image quality.11
Therefore, the operator should reduce the exposure factors whenever possible but not to the extent where useful diagnostic information is lost. It is best for operators to discuss possible dose reduction protocols with their Medical Physics Expert before putting them into practice.
Several manufacturers also allow the operator to change the voxel size. A voxel size should be chosen appropriate to the clinical question being asked. For instance, a smaller voxel size may be preferable where high detail is required. In this scenario, however, the selection of a smaller voxel size may be linked to an increase in the mA (required to reduce the noise in the reconstructed image).
Lead protection
There is no justification for the use of lead aprons during CBCT imaging. However, several studies have shown dose reduction when thyroid shields are used.12,13,14 The benefit is particularly evident for large field of view scans where the thyroid gland is close to the imaging volume, but it is unclear whether there is a significant benefit with small field of view scans. If a thyroid collar is used, careful placement is required to ensure that it does not interfere with the primary beam and cause artefacts on the image.
Reporting of Cone Beam CT scans
The complete dataset must be evaluated. It is imperative that the reporting dentist is adequately trained for this role. Small field of view scans can be reported by a dentist who has undergone further training. However, the larger field of view scans that include the sinuses, TMJs, base of skull and the cervical spine should be reported by either a dentomaxillofacial radiologist or a general radiologist with an interest in head and neck imaging (Horner Basic principles and SEDENTEXCT).15 There is British and European guidance available setting out the training requirements for dentists wishing to undertake CBCT reporting.16,17 The HPA guidance suggests an initial radiation protection training of at least 3 hours duration followed by 2 hours interpretation training with further supervised reporting of cases. The European guidance suggests a ‘Level 1’ training aimed at prescribers of 12 hours duration followed by an interpretation course (level 2 training) comprising 12 hours of theoretical training with an additional 12 hours of training in practical aspects of CBCT.
Conclusion
3D imaging is a useful adjunct to 2D imaging in selected cases. Ideally, the use of the technique should improve the outcome for the patient. It should be used in those cases where 2D imaging has failed to, or is unlikely to, provide the information required to plan treatment. If a scan is required, then the smallest volume that can answer the clinical question should be selected and the exposure factors should be optimized. The scan must be fully evaluated by a dentist or radiologist who is adequately trained to carry out the task.
