An update on local anaesthesia in orthodontics
From Volume 11, Issue 3, July 2018 | Pages 86-92
Article

Until relatively recently, the administration and use of local anaesthesia (LA) could not be counted as part of an orthodontist's routine clinical practice, particularly as procedures such as pericision and fraenectomy are relatively infrequently performed in contemporary orthodontics. With the advent of temporary anchorage devices, an orthodontist is now faced with the need to achieve adequate anaesthesia to enable their placement. Temporary Anchorage Devices (TADs) are the most common orthodontic surgically placed implants and are placed buccally between the roots of teeth in both the mandible and maxilla and also palatally in the maxilla. Less commonly, mid-palatal osseointegrated implants can be placed and are used in combination with appliances such as a palatal arch1 (Figure 1).

This article gives an overview of pain pathways and the mode of action of topical and local anaesthetics, along with providing some practical tips on their use.
Pain pathways
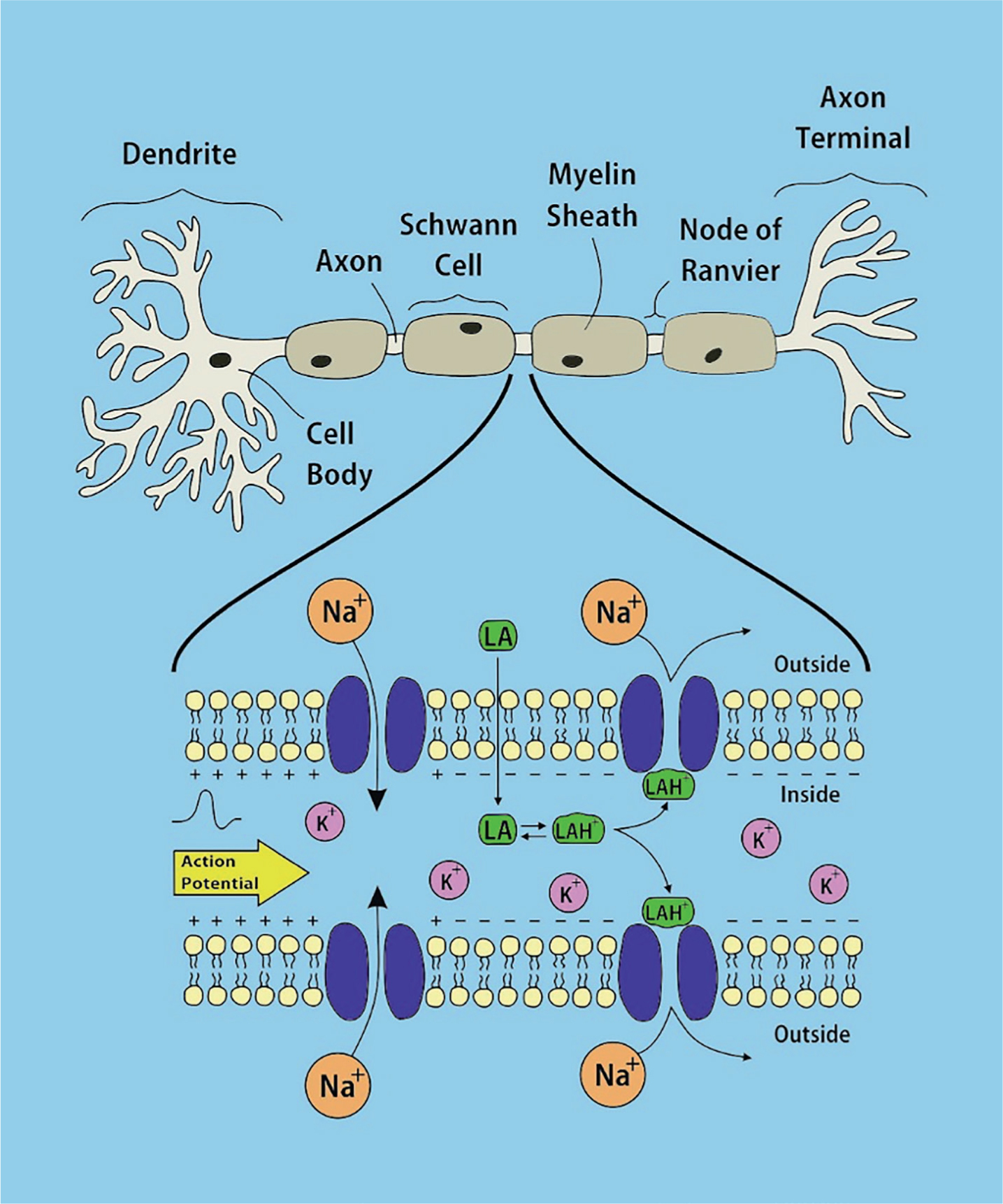
Pain is ‘an unpleasant sensory and emotional experience associated with actual or potential tissue damage’.2 It is detected via free Aδ and C nerve fibres in response to physical, chemical or thermal stimuli and the substances released following tissue damage (eg prostaglandins). Pain is transmitted by means of action potentials progressing along the nerve fibres, and is caused by the opening of sodium channels in response to depolarization, leading to a rapid influx of positively charged sodium ions into the cell. This in turn reverses the polarity and leads to the outflow of potassium ions in an attempt to restore the electrochemical gradient (Figure 2). Local anaesthesia works by entering the nerve and inactivating the sodium channels, thus preventing depolarization and the generation of an action potential.3 In this way it blocks sensory nerve conduction following nociception.
Neuroanatomy
The innervation of the dentition is derived from the branches of the trigeminal nerve (the fifth cranial nerve), which converge to form the Gasserian ganglion before entering the brain stem. Sensation to the maxilla is supplied by the second division of the trigeminal nerve: the maxillary nerve (V2). This divides into several branches, including the superior alveolar nerve (posterior, middle and anterior), the greater palatine nerve and the infraorbital nerve. Sensation to the mandible is supplied by the third division of the trigeminal nerve: the mandibular nerve (V3). The main branches that are relevant in dental anaesthesia are the inferior alveolar, long buccal, lingual, mental and incisive nerves (Figure 3).

Types of anaesthesia
There are two types of anaesthesia used in the fitting of both TADs and mid-palatal implants, namely topical and infiltrative local anaesthesia.
1. Topical anaesthesia
The placement of TADs can often be completed using topical anaesthesia4 and there are definite advantages to this approach. One of the greatest risks during TAD placement is damage to vital structures; tooth roots, nerves and blood vessels. The use of a topical anaesthetic alone can help negate this risk as deeper anaesthesia is not achieved and can allow the orthodontist to gauge sensation as the TAD is placed. If the TAD impinges on the roots of the adjacent teeth, the patient will complain of some sensitivity and the path of insertion of the TAD can be altered accordingly. However, mucosal anaesthesia alone can sometimes be inadequate as the screw penetrates bone. Indeed, the efficacy of intra-oral topical anaesthetic in dentistry has been debated with equivocal results.5, 6 Some studies have shown placement of TADs using topical anaesthesia alone to have a good overall success rate.4, 7, 8, 9 These studies used compound topical anaesthetics (CTA) comprising different anaesthetic agents (including lidocaine, tetracaine, prilocaine and phenylephrine) and in various combinations. A recent randomized controlled trial comparing topical anaesthesia and infiltrative anaesthesia during miniscrew placement found that topical anaesthesia was less predictable and could be inadequate.9 It should be noted that some of the topical anaesthetic agents used in these studies are not available in the UK. The agents currently available in the UK are Septodont Xylonor 5% Lidocaine Gel, Septodont Xylocaine 10% Lidocaine Spray and Optident Ltd Ultracare 17.9% Benzocaine Gel. More evidence is required to ascertain if these products would be appropriate for use as the sole anaesthetic agent for TAD placement.
Another advantage associated with the use of topical anaesthetic alone is avoiding the need for infiltrative anaesthesia, which is a cause of patient anxiety and reduced patient co-operation.10 It has been suggested that the use of topical anaesthesia can reduce nociception, not only through its pharmacological mechanisms, but also by virtue of a significant psychological effect.11 Many orthodontic patients have previously not experienced an interventional dental procedure, including the administration of local anaesthetic, and so a topical anaesthetic can therefore also be used prior to the use of infiltrative anaesthesia in order to reduce nociception.
A topical anaesthetic is simply a concentrated form of local anaesthetic, which is applied locally. There are a number of topical intra-oral anaesthetics discussed in the literature, including benzocaine, amethocaine and lidocaine. The more commonly used intra-oral anaesthetics in dentistry are benzocaine and lidocaine.12 There is evidence to suggest that Eutectic Mixture of Local Anaesthetics (EMLA) is effective for palatal topical anaesthesia, although not licensed and therefore not approved for intra-oral use.12
Topical anaesthetics are available in many flavours to improve tolerance, particularly in children. They are also available in a number of forms, including gels, sprays, creams, controlled delivery devices and dressings, and can be used both extra- and intra-orally. The form of topical anaesthetic preparation can alter the effectiveness of the drug, with some evidence of increased efficacy with the intra-oral use of film strips,13 microneedles14 and liposome delivery, incorporating the local anaesthetic into artificially created phospholipid vesicles.15, 16
To reach the required site, intra-oral topical anaesthetics must cross the mucosal barrier. As a result, the concentration of drug required is higher than that used in infiltrative anaesthesia, in order to ensure adequate local anaesthetic reaches the target site.12
Factors affecting the efficacy of intra-oral topical anaesthetics include the type and formulation of the anaesthetic, anatomical site, pH, concentration and time applied to mucosa.12, 17, 18 Unlike infiltrative anaesthesia, adding a vasoconstrictor has not been shown to influence the effectiveness of topical anaesthetics.19 The length of time the topical anaesthetic is applied affects the penetrative depth of the anaesthesia.20 It is therefore important that the manufacturer's instructions are adhered to in order to ensure adequate anaesthesia. The site of application also governs the degree of efficacy of the anaesthetic, with effectiveness reduced on more highly keratinized tissues (eg palatal mucosa),21 and increased effectiveness in the mandibular buccal sulcus compared with the maxillary buccal sulcus.22
The side-effect profile of intra-oral topical anaesthetics has been shown to be minimal, with the exception of cocaine, which has been associated with localized necrosis and systemic effects,23, 24, 25 and is therefore no longer licensed for dental applications. Adverse reactions include localized tissue responses or systemic reactions. The latter will be described later under systemic complications of local anaesthetics. Absorption via the mucous membranes amongst children is increased due to increased vascularity and cardiac output26 and therefore dosage should be monitored closely to avoid the risk of systemic toxicity, particularly if used in combination with infiltrative anaesthesia.
How to use topical anaesthetic preparations
Prior to using a topical anaesthetic preparation, the oral mucosa should be dried and the topical applied using a cotton wool pledget/bud (Figure 4). It has been shown that the application time of an intra-oral topical anaesthetic is important in determining its efficacy. This time can vary from as little as 10 seconds up to several minutes, depending on the product, but commonly an application time of two minutes is sufficient.12, 27

2. Infiltrative local anaesthetic
Local anaesthetics belong to one of two classes dependent on the side chain present on the active molecule. They are either amides or esters. Esters are now only used in topical anaesthetics, whereas amides are used in cartridge form for infiltrative anaesthesia. Both esters and amides have both hydrophilic and lipophilic properties, which allows them to penetrate through both interstitial fluids and the fatty nerve sheaths.28
There are many types of infiltrative local anaesthetic available and those used in dentistry include lidocaine, articaine, mepivacaine and prilocaine (Table 1). Lidocaine 2% with 1:80,000 adrenaline is a widely used local anaesthetic in dentistry and has a good safety profile. Detailed below is the maximum dosage for lidocaine in adults and children. For further information on maximum dosages please refer to the current summary of product characteristics (SPCs) from the manufacturer.
| Local Anaesthetic | Vasoconstrictor Reducing | Agent | Maximum Dose (mg/kg) | Maximum Total Dose (mg) |
|---|---|---|---|---|
| Lidocaine 2% | Adrenaline | Bisulphite | 4.4 | 300 |
| Mepivacaine 2% | Adrenaline | Bisulphite | 4.4 | 300 |
| Mepivacaine 3% | None | None | 4.4 | 300 |
| Prilocaine 3% | Felypressin | None | 6 | 400 |
| Articaine 4% | Adrenaline | Bisulphite | 7 | 500 |
Adults (18 years +)
The amount of anaesthetic administered is dependent on the procedure to be undertaken. For the placement of TADs or implants, only a small volume is usually required. However, it should be borne in mind that the maximum recommended dose of lidocaine is 4.4 mg/kg of body weight, with a maximum dose of 300 mg. A 2% solution of lidocaine equates to 20 mg/ml, or 44 mg in a 2.2 ml cartridge, hence one cartridge per 10 kg, to a maximum of approximately 7 cartridges (308 mg).
Adrenaline at a concentration of 1:80 000 corresponds to 12.5 microgram/ml or 27.5 micrograms in a 2.2 ml cartridge. The recommended maximum dose of adrenaline is 0.2 mg,29 and therefore a similar rule of 7 cartridges may be applied (0.19 mg). Care should be taken in patients with known cardiac history.
Adolescents (12−18 years) and children (4−11 years)
Special care has to be exercised when treating children. The minimum quantity of anaesthetic should be administered in order to perform the procedure adequately. The maximum dose is determined by the weight of the child. Obviously, the anaesthestic technique should be selected carefully, painful anaesthesia techniques should be avoided and the behaviour of the child during treatment has to be monitored carefully. The maximum dose for children is the same as for adults, namely 4.4 mg/kg.30
There are several components within the typical dental local anaesthetic cartridge and these include the local anaesthetic, a vasoconstrictor and a reducing agent. There may also be a carrier solution and nitrogen bubble.
The vasoconstrictor helps to reduce local blood flow and therefore increases the safety of local anaesthetic in the following ways:
A local anaesthetic solution containing adrenaline should therefore be used where possible. Where haemostasis is not a priority, the concentration of adrenaline may be reduced, 1:100 000 and 1:200 000 being available, with equivalent anaesthetic efficacy.32, 33, 34 The reducing agent (eg sodium bisulphite) helps to prevent the vasoconstrictor from becoming oxidized by reacting with any oxygen. An isotonic solution is added to reduce any osmotic effects and a small nitrogen bubble helps to prevent the presence of oxygen which could lead to degradation of the vasoconstrictor.28
As already described, there are several different local anaesthetic agents available for use in dentistry. They vary in features such as duration of anaesthesia, onset of action and efficacy. Two commonly used local anaesthetic agents in dentistry are lidocaine and articaine. There are suggestions that articaine achieves a higher success rate of anaesthesia by infiltration administration than lidocaine.35 However, either agent can be used to good effect. The maximum permissible doses of these more commonly used anaesthetics are illustrated in Table 1.
How to use local infiltrative anaesthesia
In order to administer infiltrative local anaesthesia, the mucosa should be pulled taut, the bevel of the needle placed close to the reflection of the mucosa (for a buccal infiltration) or into the palate (for a palatal infiltration) and the needle advanced until it reaches the target area. At this point, the syringe should be aspirated. If any blood is noted in the syringe, no infiltration should take place, the needle should be moved and re-aspirated. This helps to prevent administration directly into a blood vessel and thereby helps to limit any systemic effects of the local anaesthetic. In order to reduce pain, the local anaesthetic should be deposited slowly.
Local anaesthesia in the presence of inflamed tissues
Local anaesthetic is less effective in inflamed tissue. There are several mechanisms postulated to be the cause for this. The pH of the tissues is more acidic during inflammation, holding the LA in the ionized form and reducing the ability of the LA to cross the lipid membrane of the cell. The tissues are also subject to hyperaemia and therefore LA is carried away faster. There are increased levels of inflammatory factors and it is thought that these could also play a role in altered LA effects.2, 36 It is therefore important when placing TADs to avoid placement around inflamed tissues and to ensure adequate anaesthesia.
Complications of local anaesthesia
Local anaesthetics are generally very safe and effective drugs, however, there are several complications that can occur following their administration. Fortunately, while these are rarely encountered, clinicians must be aware of them. Broadly, these can be categorized as local or systemic in nature.
Local effects
Needle breakage
This is a rare complication that can usually be resolved by removing the remaining needle portion with college tweezers, where visible. If not visible, removal requires a referral to an oral and maxillofacial surgery (OMFS) unit.
Pain
The administration of local anaesthetic using infiltration may be a painful experience for the patient. Ways to overcome this include the use of topical anaesthesia, injecting the fluid slowly and ensuring that it is at room temperature at the time of administration. Anaesthetics should not be stored in the fridge, and instead should be stored at room temperature not exceeding 25°C.
Inadequate anaesthesia
This can be due to a number of reasons; variations in patient anatomy, incorrect placement, injection directly into a blood vessel, insufficient anaesthetic used, or injection into inflamed tissue.
Nerve damage
If a nerve is directly traumatized during infiltration, there is a potential for complications, including anaesthesia, dysaesthesia, paraesthesia and hyperalgesia. Fortunately, this complication is more common when using inferior alveolar (IAN) and lingual nerve blocks and these are not routinely used in orthodontics, eg during TAD placement.
Anaesthetic spread
Once again, this is a more common complication of an IAN block rather than a local infiltration during orthodontic procedures. Anaesthetizing unwanted nerves (eg the facial nerve) can occur with incorrect anaesthetic placement and can result in unwanted effects (eg facial nerve palsy − unilateral facial paresis on incorrect IAN block placement).2, 28, 37
Systemic effects
Vasovagal syncope
There is reduced blood flow to the brain secondary to vasodilation and decreased heart rate. The patient can become dizzy, pale and can temporarily lose consciousness. This is most frequently related to stress and anxiety.38 Treatment is to lay the patient flat, lift the legs and provide oxygen.39
Toxicity
Toxicity can result if too much local anaesthetic is administered. There is an increased risk of this in children and those with liver or kidney disease. Fortunately, during TAD placement the amount of anaesthetic placed should be small and not lead to a risk of toxicity. However, it is important to be aware of the risks. An overdose of local anaesthetic can have effects on both the central nervous system (CNS) and the cardiovascular system. CNS symptoms include dizziness, tinnitus, increased blood pressure and CNS depression. Cardiovascular effects include decreased contraction strength and heart rate. If an overdose is suspected, referral to hospital is recommended.2, 40
Vasoconstriction
Injection of a vasoconstrictor directly into a blood vessel can lead to increased heart rate and blood pressure. This can be avoided by ensuring to aspirate prior to injection. Blanching of areas of skin supplied downstream of vasoconstriction may be observed.
Allergy
Allergy to local anaesthetic is rare and is usually attributed to the bisulphate reducing agent, which is added to stabilize the adrenaline contained within most local anaesthetics. If there is a history of suspected allergy to local anaesthetic, a referral for allergy testing is indicated. Anaphylaxis is a rare complication and should be treated as per the medical emergencies and resuscitation guidelines.39
Fortunately, complications associated with the use of local anaesthetic administration are rare. The taking of a full medical history prior to administration is mandatory and can help avoid problems. Patients may experience more adverse side-effects with local anaesthetics if they have cardiovascular, pulmonary, liver or kidney disease, or are pregnant. It is also important to ensure that the maximum dose of local anaesthetic is considered on an individual basis.37, 40 If any serious complications are encountered, a referral to the accident and emergency department (A&E) or to the local oral and maxillofacial surgery (OMFS) team is warranted.
Summary
A knowledge and understanding of local anaesthetic agents and their delivery is important to ensure safe and effective anaesthesia, particularly with the increased use of TADs. Complications are infrequent, however, an awareness of their management is an important skill for any orthodontic practitioner considering their use.
