Abstract
In the first part of this article, the authors addressed patient-related factors that may affect the success of orthodontic treatment within the adolescent. In this second part, operator and appliance factors will be discussed.
From Volume 6, Issue 4, October 2013 | Pages 121-124
In the first part of this article, the authors addressed patient-related factors that may affect the success of orthodontic treatment within the adolescent. In this second part, operator and appliance factors will be discussed.

The operator dependent factors that might affect orthodontic outcome include:
Hospital orthodontic departments are often involved in the training of orthodontic clinicians, which may lead to any one patient receiving treatment from multiple operators. A study which looked at the effect of such practice on treatment efficiency and outcome found that, on average, treatment duration was extended by around 8.43 months as a result of multiple operators.1 Reassuringly, the standard of orthodontic treatment, as assessed by the change in PAR score, was unaffected. There do not appear to be any published data on the possible effect of the transfer of patients from one department or practice to another on the treatment duration, but it could be expected to increase both the total time in treatment and the number of appointments required to complete treatment.
There is some conflicting evidence as to whether orthodontic treatment takes longer within different clinical settings. No significant difference in treatment duration was found between similar cases within a private orthodontic practice and a university setting in Memphis, USA.2 However, in another US study, this time in Boston, treatment was found to take longer in private orthodontic practice compared with a hospital setting, even after controlling for confounding factors such as pre-treatment age, gender, race, initial malocclusion and increased number of treatment stages.3 Possible reasons for this observed difference could be related to the method of funding between the two US systems, with fees being spread over a longer time period within private practice. The occlusal outcome, measured using change in PAR scores, was judged to be similar between the two treatment settings.
The experience or grade of a hospital orthodontist has been found to be related to the total number of attendances rather than treatment duration.4 This could be due to a number of possible factors, including more efficient treatment mechanics, better time and patient management, or reduced appliance failure. An in vivo bonding study, investigating the effect of immediate versus delayed loading of brackets using postgraduate students in their first year of specialist orthodontic training, found a relatively high bracket failure rate of 14% to 17%.5 Although this study did not specifically investigate the effect of operator experience, the authors reported that this was an important contributor to the high overall bond failure rate. In a different study, designed to compare the clinical failure rates of experienced and inexperienced operators specifically, there was no reported difference in bond failure rates. This could be seen as reassuring or not, depending on one's own stage of training and clinical failure rates.6 Conversely, a recent audit within University Hospitals, Bristol found treatment duration was longer for consultants and FTTAs than with other grades of clinician. The reason for this was stated to be due to the higher caseload of patients for the more senior clinicians7 and therefore less availability of appointments. This would mean that a patient would have to wait longer to rebook an appointment if he/she had to reschedule or did not attend an appointment for any reason, leading to a longer period of appliance wear.
The experience of the operator may also influence the accuracy of the initial bracket placement on the tooth. Incorrect placement will lead to less than ideal tooth position, which will reduce the final PAR score and hence occlusal outcome. Despite the associated science of bracket design and slot placement, direct bracket positioning is often dependant upon the artistic eye and skill of the operator. One study reports an average decrease in the duration of treatment by one month when a single operator used a height gauge8 (Figure 2). Repositioning brackets during treatment may be necessary when an appliance is placed on severely rotated teeth, or teeth which have not fully erupted. They may also be repositioned in response to how the teeth move during treatment. They may also have been placed incorrectly during the bond-up procedure and it is possible that greater experience would lead to an improvement in initial bracket placement and a reduced need to reposition brackets. Alternatively, an experienced clinician may feel that early repositioning of brackets may reduce the amount of artistic archwire bending during the finishing stages. In the published literature, it is often difficult to identify when a bracket is replaced due to breakage and when it is necessary for repositioning. It could be expected that frequent repositioning of brackets could extend treatment duration but could also improve the occlusal outcome if correctly repositioned (Figure 3).

In any study of operator experience, it is important to consider the possible confounding factors, for example materials and appliances being used. In a recent survey of specialist orthodontists within the UK, it was found that operators with over 20 years' experience tended to band first molars, whilst operators with less than 10 years of experience used more bonded molar tubes.9 If banding or bonding were found to be associated with longer treatment duration or poorer occlusal outcomes, then this could lead to the incorrect conclusion that length of experience was causing the effect rather than the operator preference for banding or bonding.
When assessing appliance factors and how they might affect treatment efficiency and occlusal outcome, it is important to consider how the various components will behave in the clinical environment. Whilst laboratory tests are useful for characterizing materials, the results of such testing do not always correlate well with clinical performance.10
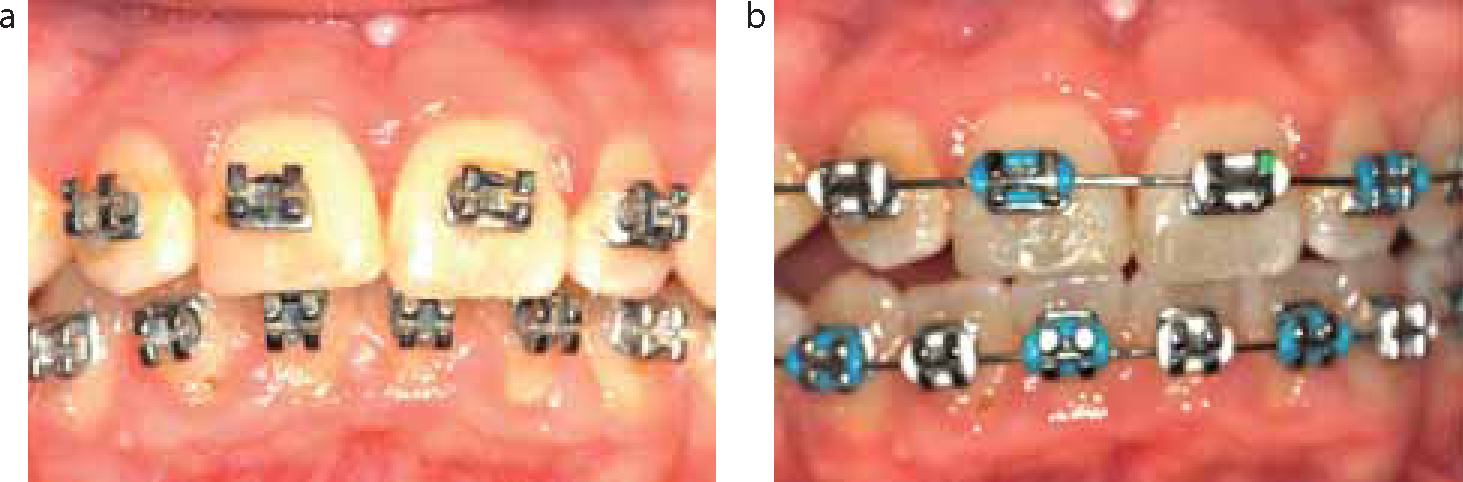
In recent years, there has been resurgence in the popularity of self-ligating brackets (Figure 4). Part of the reason for this has been the unsubstantiated theory that their use will reduce overall treatment time, as well as leading to a decrease in the total number of visits required to complete treatment. If this were to be the case, it would obviously improve treatment efficiency. However, the results of two randomized controlled trials have concluded that the use of self-ligating brackets does not lead to a reduction in the overall treatment time or in the total number of visits. Neither does their use lead to an overall greater percentage PAR reduction when compared with conventional brackets.11,12

Efficient fixed appliance therapy requires appropriate progression of archwires to facilitate the alignment of the teeth and permit space closure. A systematic review of seven randomized controlled trials compared the rate of tooth movement between patients who had received different initial archwires.13 As is often the case with such reviews, the conclusion was that the trials were judged to be of generally poor quality, although no significant difference was found in the alignment between the different initial archwires. However, in one study which looked at the total number of visits necessary to reach the final working archwires, using one of three archwire sequences found that, using 0.016” nickel titanium (NiTi) followed by 0.018 x 0.025“ NiTi and then 0.019 x 0.025” SS required only 5.7 visits for the lower arch and 5.4 visits for the upper arch. The greatest number of visits was 7.5 for the lower arch and 7.1 for the upper arch, in the case of the sequence comprising 0.016” NiTi, 0.016” SS, 0.020” SS and then 0.019 x 0.025” SS.14 Although the total duration of treatment was not recorded, it might be expected that treatments that took the most visits to reach the working archwire stages would also take longer overall to complete.
At present there do not appear to be any studies relating the choice of bonding material and duration of treatment. However, it is reasonable to assume that increased breakages associated with any particular material might lead to increased duration of treatment, and certainly to an increased number of appointments.
A systematic review of the factors affecting the duration of orthodontic treatment suggested that extraction therapy takes longer than non-extraction therapy.15 However, the evidence is based on two retrospective American studies conducted within private practice. Although there was a difference in duration between non-extraction and extraction treatment plans, it was small in both studies, being just 0.1 months in one study16 and 0.28 months in the other,17 whereas a study showing the results of 366 consecutively completed cases of one operator found extraction cases took an average of 3.3 months longer.8 The duration of treatment has also been found to be proportional to the number of teeth extracted, with treatment of patients with Class II malocclusions involving the extraction of four premolar teeth taking on average 4.6 months longer than treatment with the extraction of two premolar teeth.18 This effect is difficult to isolate from that of case complexity, since the prescribed extraction pattern will naturally reflect the initial malocclusion, in addition to the operator preferences. Thus the increased treatment duration could simply reflect a more complex case rather than the time taken to close four extraction spaces rather than two (Figure 5).

A systematic review by Mavreas and Athanasiou, perhaps not surprisingly, found that treatment with fixed appliances takes approximately seven months longer to complete than treatment with removable appliances.15 This again may be related to different presenting malocclusions and treatment objectives and differences in operator experience. In this particular study, supervised undergraduate students performed the removable appliance treatments, whilst the fixed appliance therapy was provided by supervised postgraduate students. It is certainly known that the use of fixed appliances is associated with greater improvement in PAR score and longer duration of treatment.20 In addition, dual arch fixed appliance therapy is associated with a greater reduction in post-treatment PAR score and percentage PAR change than single arch fixed appliance therapy.21
The use of additional components, such as headgear, has been found to be associated with increased treatment duration of approximately 3.66 months,22 but this increase could be confounded by increased treatment difficulty. This same reasoning might also apply to other auxiliary anchorage devices, such as Nance palatal arches (Figure 6) or temporary anchorage devices, although there do not seem to be published studies on their impact upon treatment efficiency and occlusal outcome.

The duration of treatment has been shown to increase with an increase in the number of treatment phases,22 for example two-phased treatment, such as functional therapy followed by fixed appliances to correct Class II malocclusions, increases the total duration of treatment.23 However, such treatments can lead to an overall reduction in the duration of the fixed appliance phase when preceded by the use of a functional appliance or headgear.
Although not a distinct phase necessarily, the timing of certain parts of the overall treatment will also have an effect. For example, the banding of maxillary second molars within the first 12 months of treatment can decrease the mean treatment time by almost 2 months when compared with banding the same teeth later on in treatment.8 This might be explained by the fact that, in the latter case, the alignment of these teeth is considered part of finishing rather than initial alignment, or perhaps their later alignment has almost been considered an afterthought. The same study also showed that extractions midway through treatment resulted in an additional 3.4 months of treatment compared with patients who had extractions prior to appliance placement. It would appear that the earlier these decisions are taken, the shorter the duration of treatment.
However, the evidence linking the timing of these decisions to occlusal outcome is not compelling.
As would be expected, there appears to be an association between the duration of treatment and the reduction in PAR score, as suggested by a study of board-approved orthodontists or graduate-treated cases in the USA.24 Orthodontic treatment of longer duration was shown to be associated with a greater reduction in PAR score. This is confounded by the increased chance that cases with a higher initial PAR score would be more likely to show a greater reduction in PAR score.
The factors affecting the outcome of fixed appliance therapy within the adolescent can be related to the patient, the operator and the appliance. However, it is difficult to be specific and isolate individual influences due to the multiple confounding factors. Therefore, further studies are required to confirm which of the factors are most likely to influence treatment efficiency and occlusal outcome.