Abstract
This article examines the prevalence, mechanism and risk factors associated with orthodontically induced root resorption. The long term prognosis for those who suffer severe root resorption is also discussed.
From Volume 9, Issue 3, July 2016 | Pages 96-99
This article examines the prevalence, mechanism and risk factors associated with orthodontically induced root resorption. The long term prognosis for those who suffer severe root resorption is also discussed.
External inflammatory root resorption is an inevitable iatrogenic effect of orthodontic treatment. It results in root shortening, and occurs to some extent in all patients treated with fixed appliances. For the majority of patients the shortening is minimal (< 2 mm) and causes no long term clinical problems. However, for a small percentage of patients the resorption is more severe and generalized, and has implications for the long term health and longevity of the dentition (Figure 1). The variation in the severity of resorption cannot be accounted for by different forces or mechanics used alone. There appears to be a susceptibility to resorption amongst certain patients. Recent research has focused on identifying risk factors, so patients in the higher risk categories may be made aware of this as part of the informed consent process prior to treatment.

The prevalence reported in the literature varies widely. Resorption is a 3-D phenomenon, which is difficult to quantify accurately using traditional radiographic methods. Root shortening of over 2 mm has been reported in 10–18% of patients1,2 by studies using OPT investigations. A study using histological techniques reported much higher figures of 93% of teeth showing signs of resorption following orthodontic force application for 4 weeks.3 Cone beam computed tomography has been demonstrated to be more sensitive in diagnosing resorption lesions4 and, using this technique, Lund et al reported root shortening of at least 1 mm in 94% of patients.5 In the majority of patients, resorption of less than 2 mm will be clinically insignificant, and may be accepted as an inevitable result of orthodontic treatment. Shortening of over 4 mm has been reported in approximately 6% of patients,5 and it is this cohort of patients who may have long term detrimental effects.
The most widely used index for classifying the extent of root shortening is the Malmgren index1 (Table 1). It grades the resorption from 0 to 4, ranging from no evidence of resorption to greater than 1/3 root length shortening.
| 0 | No evidence of resorption |
| 1 | Some alteration of root shape |
| 2 | Root shortening of < 2 mm |
| 3 | Root shortening of > 2 mm but < 1/3 root length |
| 4 | Root shortening of > 1/3 root length |
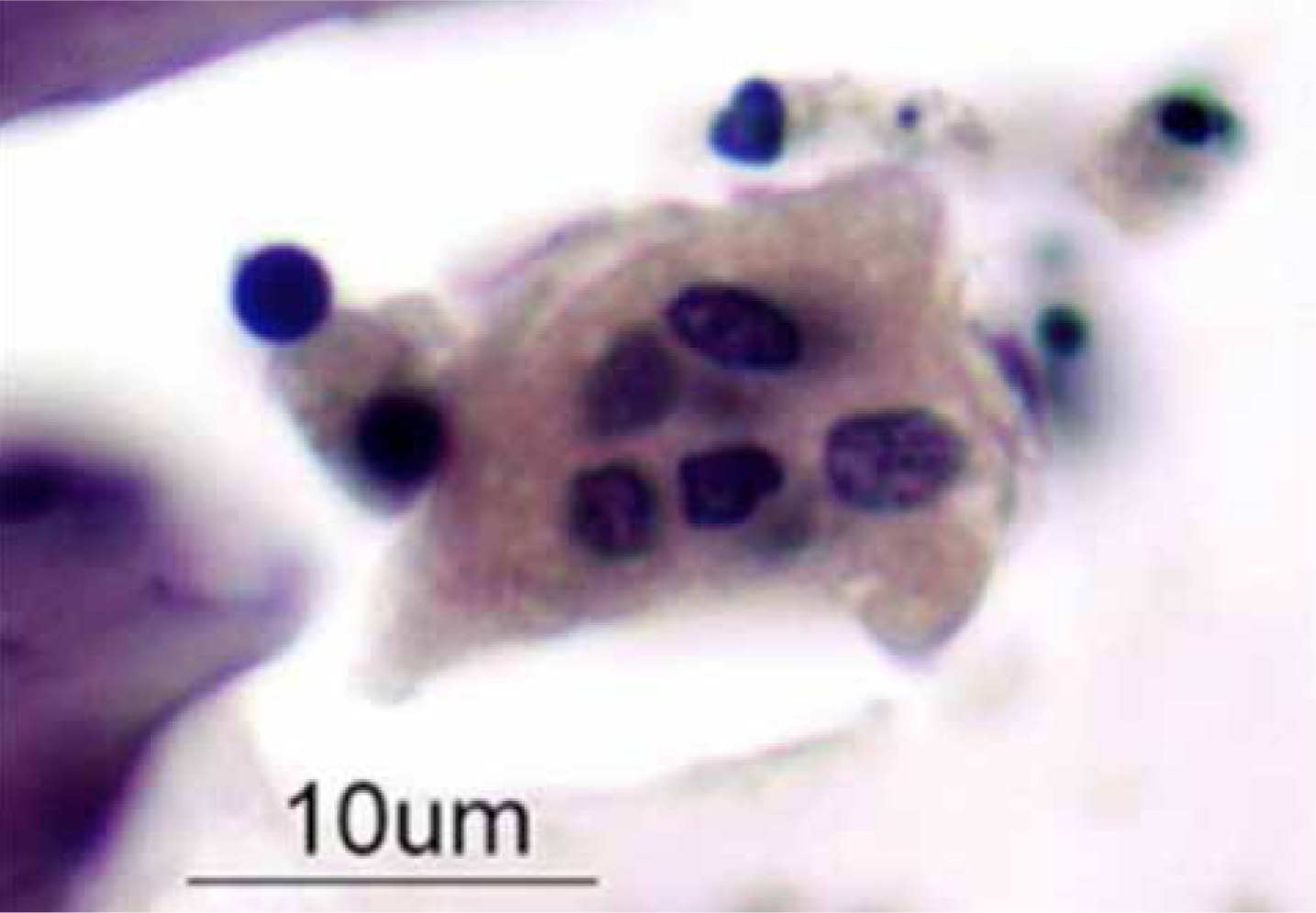
Inflammatory root resorption is a sterile inflammatory process. The cell responsible for resorption of hard tissues, either tooth or bone, is the osteoclast cell, first identified by Kolliker in 1873. It is haemopoietic in origin, meaning that it forms from the fusion of a number of precursor cells found in the bloodstream. The mature osteoclast is a large multi-nucleated cell with a diameter of approximately 40 µm and can contain up to 20 nuclei (Figure 2). Clusters of these cells are often found attached to an area of bone/tooth where active resorption is occurring. They function by creating an acidic zone in very close proximity to the hard tissue (either bone or root). This acidic environment demineralizes the tissue. The remaining organic component is then ingested by the osteoclast, and broken down by intra-cellular enzymes.
The resorption of bone is a very important physiological process which maintains bone turnover throughout life. It is also essential during orthodontic tooth movement, as bone resorption is required to allow a tooth to move in the direction of an applied force. However, if the osteoclast action occurs on the root surface, resorption will occur. The root surface is covered with a layer of cementum, which is protective and has some capacity for remodelling. If the cementum layer is removed or damaged, the resorptive process can work on the inner dentine layer. No repair or remodelling of dentine is possible and a permanent change of root shape occurs. If dentine is lost at the apex, root shortening occurs.
Damage to the protective cementum layer can occur as collateral damage following the removal of hyalinized material by macrophage or osteoclast cells.6 These cells are recruited to the periodontium when an area of hyalinization occurs, as a result of excessive force. Small areas of hyalinization are inevitable with all tooth movement. The higher the incidence of hyalinization during treatment, the greater the risk of root shortening. This is the reason why excessive forces, or longer treatment times, are implicated as risk factors for resorption.
Risk factors may be divided into patient factors and treatment factors, as shown in Table 2.
| Patient (Biological) Factors | Treatment (Mechanical) Factors |
|---|---|
| Genetic susceptibility (IL-Iβ gene) | Fixed appliances |
| Systemic disease | Extent of movement |
| Age | Intrusion of teeth |
| Gender | Intermaxillary traction |
| Habits | Increased treatment time |
| Tooth structure | Rectangular archwires |
| Previous resorption |
Several studies have indicated that there is a genetic contribution to susceptibility to resorption. A twin study indicated phenotypic concordance for 49.2% of monozygotic twins and 28.3% of dizygotic.7 While this indicates a genetic component, the fact that the monozygotic concordance was not 100% confirms environmental factors also play a role. The IL-1β gene has been linked to the aetiology of resorption, with one study showing those patients homozygous for the IL-1β allele are over 5 times more likely to develop root shortening of over 2 mm.8
Hypothyroidism, pituitary disorder and hyperparathyroidism have been implicated in increased levels of resorption.9 These hormones are important in the regulation and control of bony remodelling. Medications including L-thyroxine and corticosteroids have been shown to decrease resorption levels in rats.
Resorption is seen to be more prevalent in adults compared to children. This may be explained by the fact that adult bone is more dense and less vascular, and there is a narrower periodontal ligament space. Therefore, undermining resorption can occur more commonly in adults, leading to increased root resorption. It has been reported that females are more at risk of developing resorption,10 but this is not accepted by all.2 The reported increased risk to pipette-shaped roots has also been questioned by a more recent study.11 It has been shown that teeth which have been successfully endodontically treated are not at a higher risk of resorption. Neither are teeth which have suffered trauma at a higher risk, unless they demonstrated previous resorption associated with the traumatic injury.12
During bodily movement of a tooth, the force is evenly distributed along the root and bone is theoretically only resorbed by frontal resorption. Therefore, it has been suggested that bodily movement with fixed appliances should result in less resorption than tipping movements. However, Linge and Linge found that patients treated with rectangular archwires had an average of 0.4 mm more root shortening.2 In reality, due to the slope within the bracket, and the action of frictional binding, all tooth movement with fixed appliances involves an element of tipping. It is not achieved purely by frontal resorption of bone. The higher force levels exerted by fixed appliances, particularly when using rectangular archwires, also contribute to the increased resorption levels. It was also shown in this 1983 study that patients treated with fixed appliances for over 15 months were at a higher risk of resorption.
Informing the patient of the risk of resorption during the consent process is extremely important. If any patient risk factors have been identified, these should be explained and discussed prior to embarking on treatment.
Comments on root lengths, and any existing pathology, should be made in the patient notes. If there are any indications for undertaking progress radiographs 6 months after commencing treatment, this should be explained to the patient. There should be a clear plan for what will be done should the progress radiograph indicate resorption is occurring, for example halting active treatment for a number of months.
The pathological process will stop once treatment ceases and therefore, once severe resorption is identified, the extent of further tooth movement should be minimized, if possible. This may require some compromise in the attainment of the ideal treatment goals. There is some evidence that stopping active tooth movement for a period of 3 months is beneficial,1 but the decision to do this must be made taking other risks into account, for example the risk of demineralization if oral hygiene is not optimal.
Happily for clinicians and patients, teeth which suffer severe root shortening during treatment demonstrate a good long term prognosis, and the resorptive process has been shown to cease once orthodontic tooth movement is complete. A retrospective study examined 100 patients 14 years following treatment completion, and found no tooth loss had occurred as a result of the resorption.11 Patients must be educated as to the importance of long term oral health, as any bone loss due to periodontal disease is to be avoided. Teeth which have suffered severe resorption may not be suitable for fixed prostheses, such as crown or bridgework, due to the unfavourable crown-root ratio.
Orthodontically induced root resorption is inevitable in all patients treated with fixed appliances. However, there is a small minority of patients who will suffer severe root shortening. It is important to bear this risk in mind when planning treatment, and explain it thoroughly to the patient as part of the informed consent process. Patient-related risk factors, including genetic susceptibility, are the subject of ongoing research, and it may be possible in the future to predict accurately who is likely to develop severe resorption. It is important to minimize mechanical risk factors, such as heavy forces, with all patients. Should patients develop severe resorption, they may be reassured that the teeth have a good long term prognosis and the pathological process is likely to cease when orthodontic treatment does.