Abstract
This paper presents a series of five cases in which the mandibular second premolars have taken a different path from normal development. The current literature has been reviewed and the management of these teeth described.
From Volume 6, Issue 2, April 2013 | Pages 38-43
This paper presents a series of five cases in which the mandibular second premolars have taken a different path from normal development. The current literature has been reviewed and the management of these teeth described.

Mandibular second premolars usually erupt between 11 and 12 years of age. They are described as being highly variable in the timing of eruption and developmental position. The most prevalent malposition reported is distal inclination.1 Usually, this disto-angular position corrects as the developing tooth erupts.2 They are one of the last mandibular permanent teeth to erupt and often demonstrate significantly retarded development, especially when at least one permanent tooth is absent.3,4 Owing to its relatively late stage of development, it can become displaced or impacted in crowded arches. Nearly 2% of European population samples have one or both mandibular premolars developmentally absent.5
There are a number of possible outcomes associated with unerupted mandibular second premolars. This paper presents a series of five cases in which the tooth or teeth have taken a different path. The literature has been reviewed and the management of these teeth described.


A 25-year-old female presented with a Class I malocclusion with all permanent teeth erupted except for the upper left permanent canine (UL3), the lower left second premolar (LL5) and all third molars. The upper left deciduous canine (ULC) was retained and not mobile and the UL3 was ectopic and palpable palatally. The patient's main concern was the appearance of the retained ULC. She described a history of early loss of several deciduous teeth as a child. There was no relevant medical history.
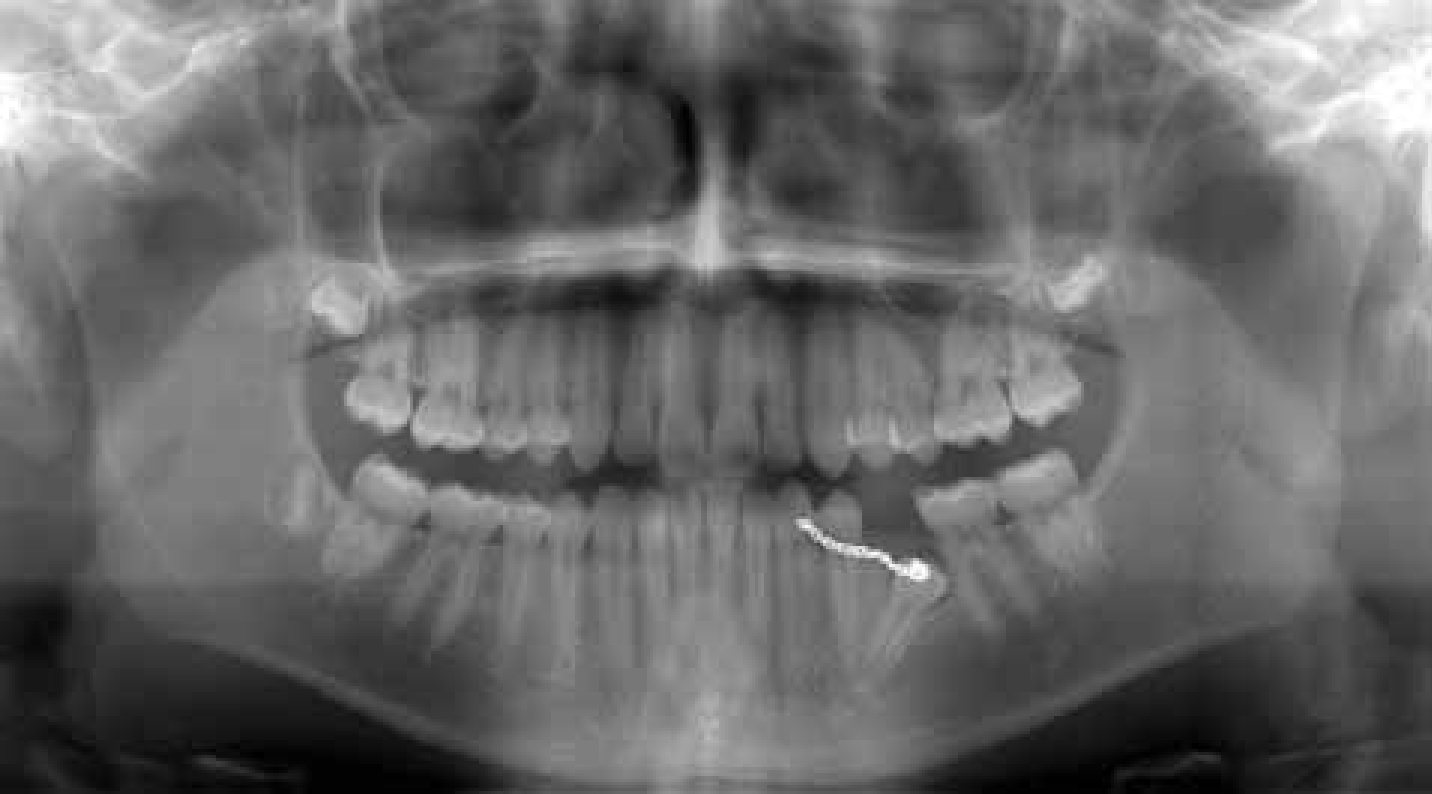
The OPT showed the UL3 to be palatally positioned and the LL5 to be impacted (Figure 1). A treatment plan was agreed with a view to extracting the retained ULC and LLE followed by a course of upper and lower fixed appliance treatment to open spaces for the impacted teeth to erupt. The UL3 started to erupt within 6 months of extraction of the deciduous canine and placement of fixed appliances. A second OPT (Figure 2), taken 9 months after the start of fixed appliance treatment, showed no significant improvement in the position of the LL5, and surgical intervention with an open exposure was agreed to allow orthodontic traction to the tooth. The tooth was aligned and the fixed appliances debonded after 25 months in active treatment. Retention involved upper and lower vacuum-formed retainers worn at night-time.
Lower second premolars are the third most commonly impacted teeth after third molars and maxillary canines, and have been found to be involved in 24% of all impacted teeth, excluding third molars.6,7 An impaction of a lower second premolar can occur as a consequence of:
Pathological sequelae as a result of this impaction are:
There are numerous treatment options available for the impacted mandibular second premolar:

The treatment option chosen is dictated by several factors. These include the developmental stage of the tooth, age of patient, its position, general oral health, the malocclusion, proximity of adjacent structures and the patient's individual preferences and motivation towards treatment.


A 13-year-old girl was referred for the management of mild hypodontia and an ectopic and horizontal lower right second premolar (LR5). She presented with mild Class II division 1 malocclusion on a mild Class II skeletal base with average vertical dimensions. The upper left deciduous incisor (ULB) was retained and the upper right lateral incisor (UR2) was peg-shaped. The lower left and lower right second deciduous molars (LLE, LRE) had been extracted 4 months before presentation. An OPT was taken which showed the upper left lateral incisor (UL2) to be developmentally absent, and the LR5 to be late developing, with abnormal horizontal position of the tooth bud in relation to the mid-sagittal plane. An OPT taken 6 years previously showed the LR5 to be absent, while the tooth bud of the second premolar on the contra-lateral side was seen to be developing.
The treatment options were explored with the patient, and it was decided to extract the diminutive UR2 and ULB. An upper fixed appliance was placed to close the lateral incisor spaces with a view to monitoring the development and position of the LR5 over 12 months. If the tooth failed to erupt, the options available were whether to leave and monitor, or extract, the tooth in the longer term. The risks associated with removing the tooth included damage to the adjacent teeth and the mental nerve during surgery. The resulting space could be accepted or restorative options could be considered, such as a bridge or implant, once growth is complete.
Although both genetic and local environmental factors can influence the normal eruption of teeth, accumulated evidence suggests that mandibular second premolar malpositions are often related to a broader genetically related pattern of dental anomaly. They often show significantly retarded development, especially when at least one permanent tooth is absent (as seen in the case above).3,4 Delayed tooth formation has been reported in children with clefting, palatally displaced canines and with malposition of mandibular second premolars.11,12,13,14 A ‘late bud’ has been defined as a permanent tooth which does not follow a biologically established sequence and whose development is delayed by at least two or three years.15
Second premolar calcification usually begins between 24 and 30 months of age. However, it is not uncommon for mandibular second premolars to calcify as late as 5 years of age.16,17 It is therefore prudent to monitor dental development and assess the degree of tooth formation in the contra-lateral quadrant. A slow, asymmetrical development of the contra-lateral second premolar may alert the clinician to possible aplasia of the tooth.
An exaggerated disto-angular malposition of the unerupted mandibular second premolar has been associated with agenesis of its antimere.11 Both agenesis and clefting have been shown to be associated with the mandibular second premolar malposition anomaly.18,19 The homeobox gene MSX1 is associated with both agenesis and with clefting.20,21 Distal inclination of the unerupted premolar and retarded formation appear to be two different but regular features in genetically controlled dental anomaly patterns.22 It is important for dentists and orthodontists to be aware that associations between certain dental anomalies exist to allow early detection of any significant disturbances to tooth position, number and formation. This knowledge, together with clinical experience that such teeth usually self-correct and erupt given time, will reduce active intervention in cases where a more passive approach of monitoring is preferable.


A 14-year-old boy was referred for advice and treatment by a specialist orthodontist. He presented in late mixed dentition with a developing Class II division 1 malocclusion. The lower left second deciduous molar (LLE) was severely submerged and the underlying second premolar was immature and horizontally positioned (Figure 7). Extraction of the submerging deciduous molar was advised. The patient was reviewed 16 months later, and it was noted that the ectopic lower second premolar had uprighted and erupted into the arch. An OPT shows the root to be less well developed when compared to the contra-lateral second premolar (Figure 8).
Clinical experience shows that such teeth often self-correct and erupt given time, which can alleviate the need for active intervention in cases where a more passive approach of monitoring is preferable.




A 14-year-old boy with no relevant medical history was referred by his dentist for advice and treatment. His main concern was the appearance of the midline diastema. He presented in the late mixed dentition with a Class II division 1 malocclusion on a mild Class II skeletal base with average vertical dimensions. The overjet was increased at 9 mm and the overbite increased and completed on to the palatal mucosa with no obvious trauma. The molar relationship was half unit Class II bilaterally. The upper arch was spaced, and the lower arch severely crowded in the lower left permanent canine region. The upper right second deciduous molar (URE) and lower left and lower right second deciduous molars (LLE, LRE) were retained.
The upper right and lower right second premolars (UR5, LR5) were ectopic (Figure 9). The UR5 also appeared diminutive. Arrangements were made for the patient to have extraction of all retained second deciduous molars, with a view to monitoring the unerupted and ectopic second premolars. The patient had a course of functional appliance therapy with Clark twin block appliances to reduce the overjet and improve the molar relationship. The UR5 erupted into the mouth during the functional appliance phase and a decision was made to maintain the tooth, despite its morphology being diminutive with a less well developed root.
The patient was booked for closed exposure with a gold chain to allow orthodontic traction to the LR5 at the start of the fixed appliance stage, which had originally been planned with an upper appliance only until the fate of the lower right second premolar could be decided. Unfortunately, the patient failed to attend several surgical appointments, and a new radiograph taken over 18 months after the initial diagnostic appointment showed the LR5 to have improved in position (Figure 10). At this stage, the patient expressed reluctance to have lower fixed appliance treatment and the tooth was left to erupt. A periapical radiograph (Figure 11) of the LR6 taken at the end of treatment showed resorption of the mesial root, and bony infill of the resorptive defect. The tooth gave a positive response to vitality tests, and a decision was made to monitor this tooth with no intervention. Figure 12 shows eruption of the LR5 into the mouth.
Resorption of mandibular molars by second premolars is not a common occurrence, and only two cases have been reported in the literature.8 The mechanisms by which teeth cause root resorption are unclear. It has been suggested that cytokines secreted by reduced enamel epithelium and the dental follicle of the impacted tooth may cause osteoclast recruitment, connective tissue destruction and root resorption.23 It is difficult to predict whether an impacted tooth is likely to be associated with pathological changes. Case 4 highlights the importance of identifying potential risks of unerupted impacted teeth, and the importance of monitoring the teeth clinically and radiographically. This case also demonstrates the eruptive potential of ectopic second premolars, once space has been created for the tooth.


A 12-year-old boy was referred by his dentist for an orthodontic assessment and management of impacted upper left and upper right permanent canines (UL3, UR3), and bilateral impaction of lower second premolars. There was no relevant medical history.
The patient presented with a Class I malocclusion with severe upper and lower arch crowding. The lower left second deciduous molar (LLE) was retained but mobile. An OPT (Figure 13) showed all permanent teeth to be present. The UL3 and UR3 were ectopic and slightly palatal, the lower right second premolar (LR5) was impacted and in line with the arch, and the lower left second premolar (LL5) was ectopic and at approximately 45° to the mid-sagittal plane with the crown directed towards the border of the mandible.
The patient was not keen to pursue active orthodontic intervention, and a treatment plan was agreed with a view to extracting the upper left and upper right and lower right first premolars (UL4, UR4, LR4), as well as the LLE. A decision was made not to remove the ectopic LL5 owing to its proximity with the roots of the first permanent molar and inferior alveolar nerve. The plan was to review the patient in 12 months to assess the position of the impacted teeth and ectopic LL5. The UL3, UR3 and LR5 all erupted uneventfully. The patient failed to attend numerous appointments, but returned to the department 10 years later at 21 years of age. An OPT taken at this stage revealed the lower left second premolar to have migrated across and below the roots of the molar teeth and was situated distal to the lower left third molar tooth. There appeared to have been some root resorption to the first and second molars. The patient was not experiencing any symptoms and there was no radiographic evidence of any cystic changes to the unerupted premolar. No active intervention was carried out. An OPT (Figure 14) taken 19 years after initial presentation (at 31 years of age) shows the LL5 to be ascending the ramus of the mandible towards the coronoid process, with no symptoms or pathological signs seen radiographically. A decision was made not to intervene.
‘Transmigration’ is the term used to describe ectopia when a tooth or teeth are present in areas distant from the alveolar process.24 Case 5 illustrates how the disto-angular mandibular second premolar can migrate distally across the mandibular body, below the molar roots, and become irreversibly impacted. It has been suggested that transmigration has a genetic origin, and has been associated with other developmental anomalies, such as hypodontia, diminutive lateral incisors, palatally displaced canines and bilateral occurrence of this anomaly.25,26 When this occurs, active intervention is not always advisable as the risks associated with surgical intervention (damage to adjacent structures, active intervention requiring a general anaesthetic) often far outweigh the risks associated with leaving it in situ and monitoring it long term. Transmigration is not a common finding, and there are few reported cases in the literature, most of which are of mandibular cuspids not bicuspids.26,27,28,29,30,31
Orthodontists are involved in the management of the developing dentition. They are trained to assess and treat malposition anomalies. Although orthodontic treatment planning is primarily based on clinical and radiographic assessment of patients, advances in technology have also given us the option of three-dimensional imaging, such as cone beam computed tomography (CBCT). CBCT may allow better localization of impacted teeth and any associated root resorption more accurately. It is not indicated routinely for all cases as the radiation dosage involved can be considerably higher than conventional two dimensional imaging.32 However, in some complex cases requiring multidisciplinary management, three dimensional imaging can provide valuable additional information which may influence treatment planning.
When a patient presents with an ectopic mandibular second premolar, delayed development, root resorption or a variation from ‘normal’ development, it is essential that, as clinicians, we are equipped with the knowledge to be able to make sound clinical judgements based on the evidence.