Abstract
Data was collected retrospectively from 44 patients who had orthognathic surgery between May 2012 and October 2014. Treatment was completed by a single consultant surgeon and three orthodontists.
From Volume 9, Issue 2, April 2016 | Pages 59-62
Data was collected retrospectively from 44 patients who had orthognathic surgery between May 2012 and October 2014. Treatment was completed by a single consultant surgeon and three orthodontists.
Patients undergoing combined orthodontic and orthognathic surgical treatment constitute up to 7% of a UK-based orthodontic consultant's caseload.1 Patients wish to know duration of treatment. Therefore, each unit needs awareness of average treatment times to inform patients better and thus improve the consent process and patient-centred care. Owing to the prolonged and involved nature of this treatment, requiring numerous hospital visits, patients are keen to have as accurate an idea as possible as to the duration of treatment.
The process we are most familiar with today involves pre- and post-surgical orthodontics, with surgery performed once teeth have been suitably aligned and decompensated. Post-surgical orthodontics involves finishing and perfecting the occlusion, a process which is not possible by surgical movements alone.
Cases involving combined orthodontic and orthognathic treatment are most commonly treated in a hospital setting because of the multidisciplinary care necessary for their management. The complexity of treatment also has an affect upon the duration of treatment, and it is therefore important to have an average duration of treatment for the particular treating department as times may vary from those quoted in the literature and thus quoted to patients during consultation and treatment planning.
This audit was carried out to assess whether the department was meeting appropriate standards, and whether the information given to patients about treatment duration was correct, thus enabling an improved consent process for patients where the treatment plan involves combined orthodontic and orthognathic surgery treatment.
It was stated to our patients that treatment would take approximately 2.5 to 3 years (30 to 36 months). As patients often remember the shortest duration quoted, the standard was set at 2.5 years (30 months). 100% of patients should ideally complete treatment within the estimated duration (2.5 years) as stated during the consent process. This is the same standard as was set by a similar study completed in NHS Tayside.
Data were collected retrospectively from 39 patients who had orthognathic surgery between May 2012 and October 2014. Orthodontic treatment was completed by three consultant orthodontists at hospitals across NHS Lanarkshire. Surgery was completed by a single consultant maxillofacial surgeon at Monklands Hospital.
Data were recorded in a data collection table including the following criteria:
The duration of the various stages of treatment was recorded: duration of pre-surgical orthodontics; waiting time from final joint clinic appointment to surgery; duration of post-surgical orthodontics and the total treatment duration. Duration was measured in months, based on the assumption that there are 30 days in one month.
The end of pre-surgical orthodontics was judged as the time of the last joint clinic, where that surgeon and orthodontist are present to decide whether the patient is ready for surgery and to give a provisional date for surgery. Owing to the combined nature of this treatment, this seemed the most reliable time and does reflect the importance of both groups of consultants assessing the patient. Previous studies have used the date of the last orthodontic adjustment as the end of pre-surgical orthodontics. This may present inaccuracies as the patient may have been ready for surgery but there was an elective delay due to patients' other commitments. Furthermore, if there is a long waiting time for surgery, the patient may attend for an orthodontic appointment to retie wires and make minor adjustments to ensure that nothing moves unfavourably prior to surgery, which would appear to lengthen the duration of pre-surgical orthodontics.
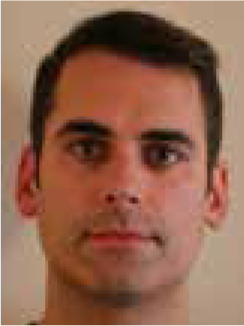
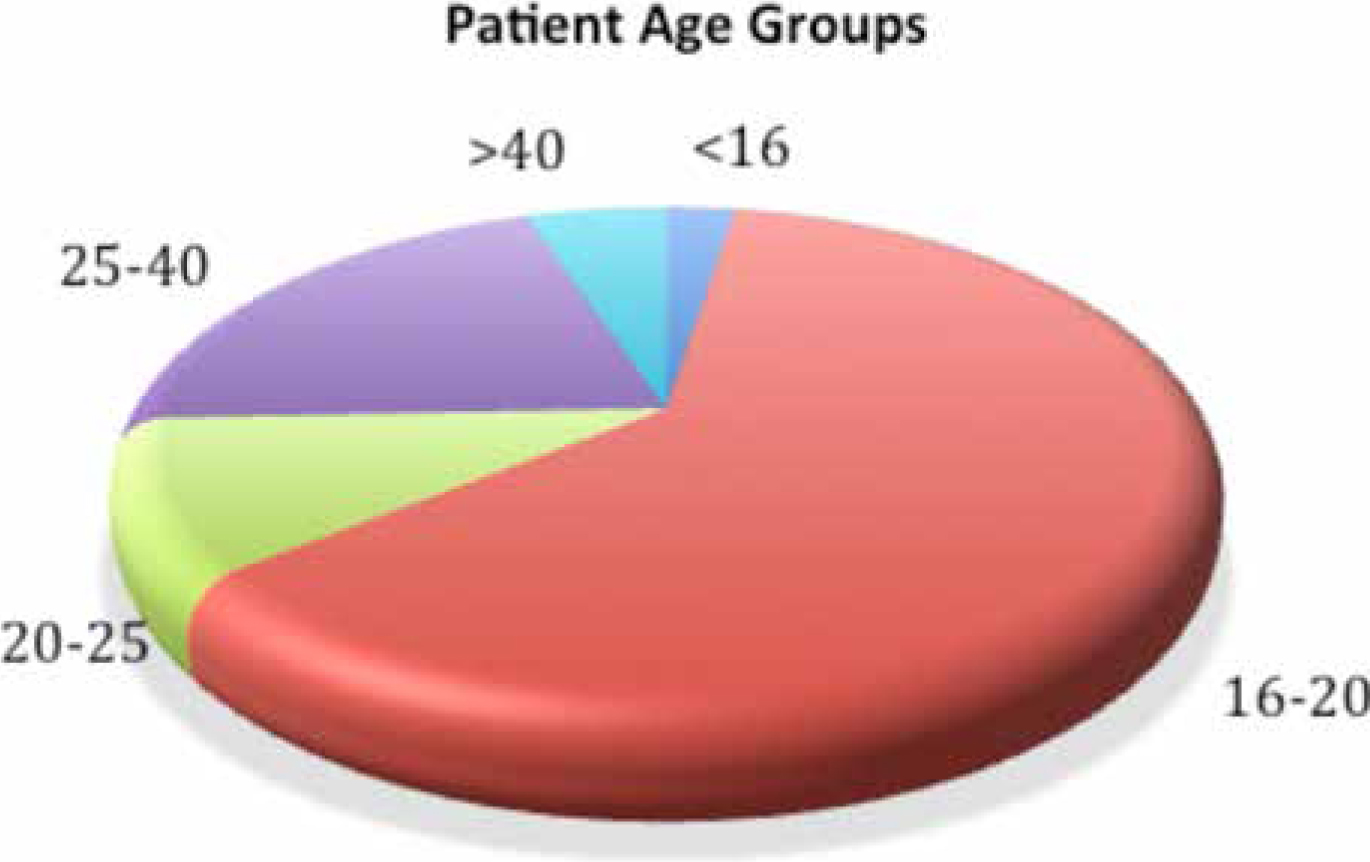
This patient cohort comprised 18 males and 21 females. Of these, one had a Class I malocclusion, requiring correction of a 5 mm anterior open bite, 11 were Class II division 1, 5 were Class II division 2 and 22 Class III (Figure 1). The average age at the start of pre-surgical orthodontic treatment was 21.9 years (Figure 2). Out of the 39 patients treated, 5 had mandibular surgery only, 7 had maxillary surgery only and 27 had bimaxillary procedures.
The mean total duration of treatment was 29.4 months, which is marginally better than the set standard of 30 months (Figure 3). The range of duration was 17.8 to 57.3 months (standard deviation 8.4). However, only 59% of patients completed within 30 months, thus indicating that the standard was not being met with a large proportion of patients. However, 82% of patients completed treatment within 36 months, which is the higher end of the quoted treatment duration.
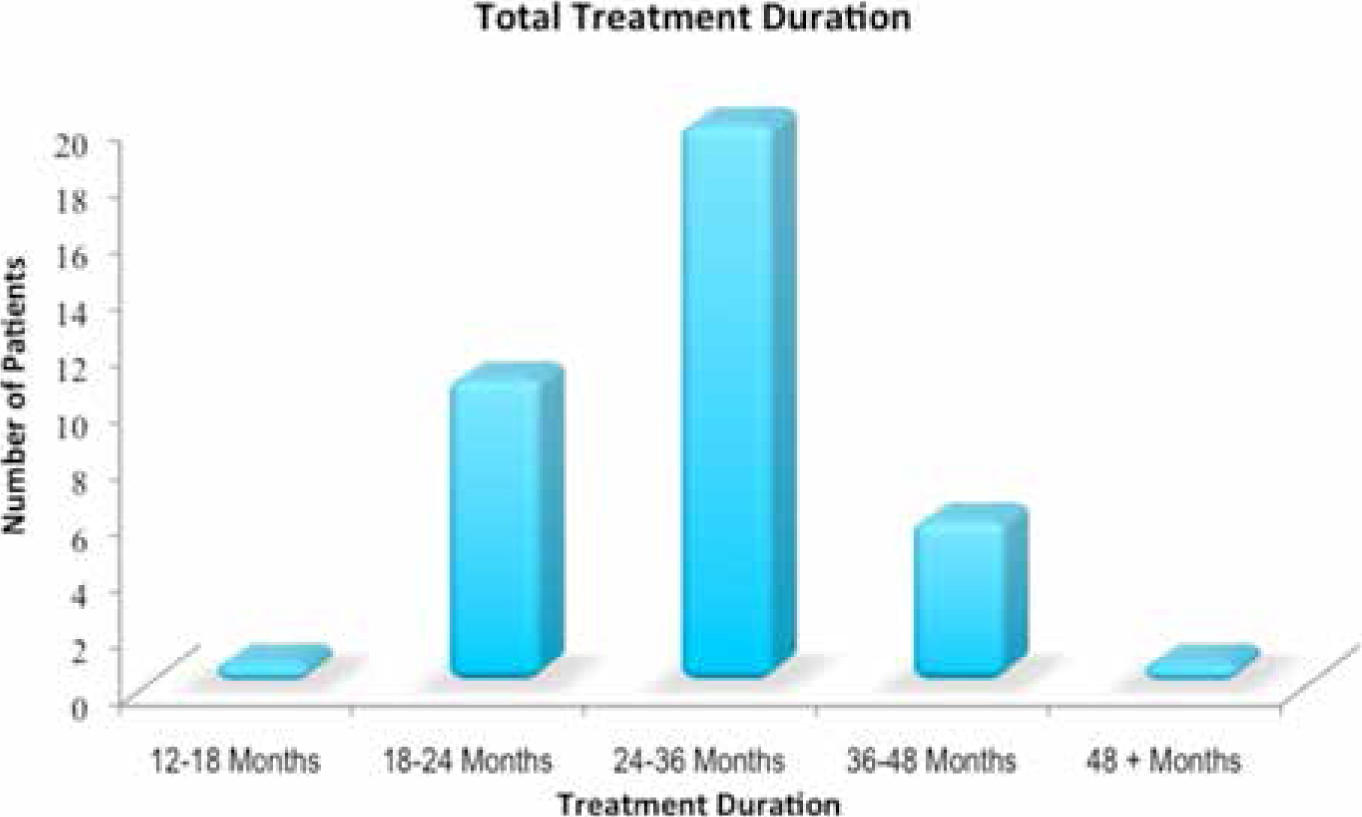
The mean treatment durations of the various treatment stages were (Figure 4):
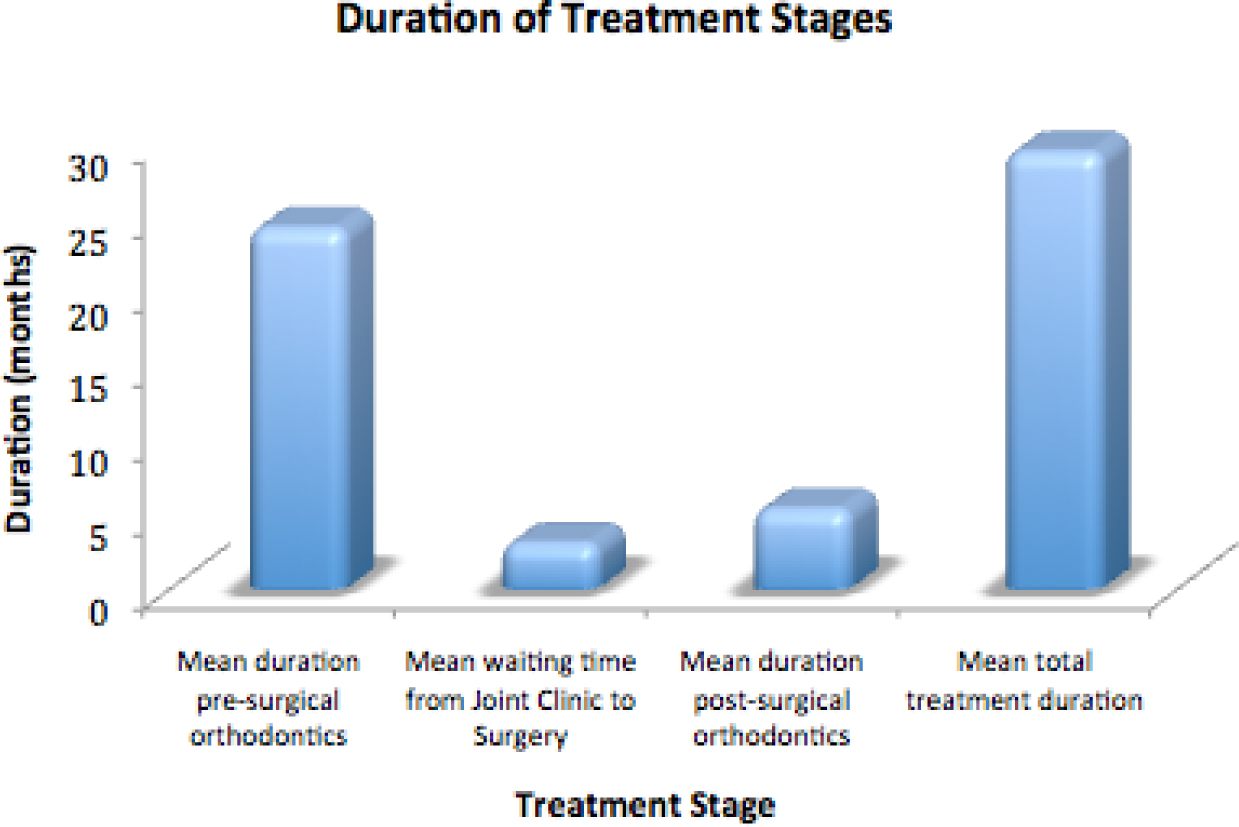
The mean overall treatment time was 29.4 months. This is slightly lower than those figures previously reported in similar studies.1,2,3,4,5 Arad et al quote a mean duration of treatment of 30.6 months.2 The longest treatment stage contributing to a mean duration of 29.4 months is the duration of pre-surgical orthodontics, as found in other studies.1,2,3,4,5 Pre-surgical orthodontics duration of 24.3 months is similar to that found by Dunbar et al1 and Jeremiah et al,3 but significantly longer than the studies by both Luther et al4 and Dowling et al.5 However, it was noted by Dunbar et al1 that a large proportion of the orthodontic treatment was carried out by orthodontic trainees, which may have accounted for longer than predicted treatment duration. Nevertheless, all treatment in NHS Lanarkshire was performed by an orthodontic consultant.6 Post-surgical orthodontics duration of 5.4 months is shorter than the studies by Dunbar et al,1 Jeremiah et al,3 Luther et al4 and Dowling et al.5 Class II malocclusions take longer to treat than Class III (29.5 months vs 27.8). Le Fort I osteotomies treatment duration is significantly shorter than for both mandibular and bimaxillary surgeries (26.2 months vs 31 and 31.2 months, respectively), as found by Arad et al.2 Fifty-nine percent of patients completed treatment within 30 months. This is significantly lower than the standard set of 100% of patients to complete treatment within 30 months, as quoted during the joint clinic and consent process. However, 82% of patients do complete treatment within the higher quoted duration of 3 years/36 months. It should also be mentioned that there was a changeover of surgeon in May 2012, and there was a period of 4 months with no surgeon in post, thus lengthening treatment duration, mainly in the waiting time for surgery stage.
It has been suggested that adopting a surgery first approach to combined orthodontic and orthognathic surgery treatment may reduce overall treatment time.7 This method was discussed in 1977 by Epker and Fish, who highlighted advantages to performing surgery first, namely: an improvement in aesthetics and function early in treatment rather than over a number of years; improvement in swallowing and speech functions post-surgery; faster tooth movement post-surgery thus reducing orthodontic time; improved patient co-operation with orthodontics and easier tooth movement due to introduction of both normal functional and anatomical relationships post-surgery.8 Huang et al's systematic review concluded that a surgery first approach had a significantly shorter treatment duration whilst maintaining similar long term stability to the more traditional orthodontics first approach.7 However, it also admits that further studies are required to provide further clinical evidence to support this view, as currently published studies involved mainly correction of Class III malocclusions and do not include the other dento-facial anomalies treated with combined orthodontic and orthognathic surgery treatment.7 Significant disadvantages with a surgery first approach have also been discussed, including high bonding failure, difficulty in placing the surgical wire on certain malocclusions, greater surgical movements required to compensate for post-surgical orthodontic movements and occlusal instability.9
When comparing studies, differences which may have an impact on treatment duration must be taken into account, such as: private vs public health care systems; grade of clinician (ie whether trainees are involved in treating); as well as how the stages of treatment are measured.
Estimates of treatment duration should be as realistic as possible when discussing and giving consent to patients for combined orthodontic and orthognathic surgery treatment. Aspects that could alter treatment duration should be identified and these should be addressed at both initial assessment and when giving consent to patients for treatment.
These results show that 59% of our patients undergoing combined orthodontic and orthognathic surgery treatment complete treatment within 30 months/2.5 years and 82% within 36 months/3 years. This higher figure should therefore be quoted when giving consent to patients for treatment, to avoid raising patient expectations.
The impact of surgery on a patient's life must not be underestimated and ensuring that surgery is at a time that is of minimal disruption to the patient is paramount to patient-centred care. This is an inevitable factor out of the practitioner's control that will often affect treatment times, particularly the time from completion of pre-surgical orthodontics to the date of surgery.
It can be seen from the aforementioned studies that the most significant contribution to treatment duration is pre-surgical orthodontics. This time, however, is difficult to compare and assess owing to the lack of clarity when the patient is officially ready for surgery. There should therefore be regular communication between orthodontist and surgeon to decide when a patient is ready for surgery so that it can be recorded when pre-operative orthodontics is complete. It would be useful to ensure consistency across the departments by introducing record-keeping proformas to assist in the collection of the required information. In addition, waiting times for a joint clinic appointment when only one surgeon is available, as in this study, will obviously have an affect on this treatment duration stage.